 Today at 9:30, Claire and I arrive at Dr. Lerner’s office for chemotherapy treatment number 5. The plan, as on previous treatment days, is that Claire will wait with me until my consultation with the doctor is finished, then will leave me there, returning at the end of the day when the treatment is finished.
Today at 9:30, Claire and I arrive at Dr. Lerner’s office for chemotherapy treatment number 5. The plan, as on previous treatment days, is that Claire will wait with me until my consultation with the doctor is finished, then will leave me there, returning at the end of the day when the treatment is finished.I go back for the insertion of the needle into my porta-cath, and for the drawing of blood for my weekly blood test (which, on chemo days, is ordinarily done right through the porta-cath). This time, though, there is some difficulty with some kind of clotting or residue that’s keeping the porta-cath from working properly. Raquel, the nurse, injects something into the porta-cath that will dissolve whatever it is that’s clogging the device. This medication will take about a half hour to do its work, so Raquel has one of the phlebotomists come in to draw my blood sample through the arm – the usual procedure on non-chemo days. It’s a second needle stick, but I’ve gotten so used to blood tests by now that it doesn’t trouble me at all. I hardly feel it any more.
My blood count, again, is just fine. White cells are below normal, but not by much. No one seems overly concerned about that.
Claire joins me, then, and we go in to see Dr. Lerner. He asks about my problems with nausea, and I tell him that the combination of Emend and Kytril – two oral anti-nausea medications – seemed to have helped last time, so he prescribes those again this time around. We talk about fatigue, and how exercise is part of the solution to that. It’s something of a vicious cycle – it’s hard to exercise when you’re feeling weak, but, paradoxically, exercise is something that helps build strength. At the cancer fatigue seminar this past Monday, I had heard Marcia, a physical therapist from Life Fitness – the hospital-owned fitness center where I used to work out – talk about the things they can do for cancer patients. I mention this to Dr. Lerner, and he makes arrangements for someone from the Cancer Navigator support program at Ocean Medical Center to call me, and see if this would be a possibility. I’m hoping that - since the doctor's prescribing it - my medical insurance can offset the cost, but even if it doesn’t, I’ll probably do it anyway. I feel I need to do something to get active again.
I ask for more information about the radiation treatments, and Dr. Lerner tells me a bit more, Last time he described it as “a possibility,” but this time he says it will be a virtual certainty, given the sort of bulky tumor I’ve got. He says he will probably be referring me to Dr. Nathan Kaufman, who’s chief of radiation oncology at Ocean Medical Center. Dr. Lerner will continue to direct my overall treatment, but Dr. Kaufman will plan and administer the radiation. Those treatments will probably be five days a week for three weeks, beginning a few weeks after my last chemo treatment.
 I go in for the chemo at about 10:30, which lasts until about 5:30. The medicine has done its work, unclogging the porta-cath, so everything proceeds as on previous occasions. The office is evidently crowded today, so for the first time I get a roommate in my little cubicle: a retired woman who’s there for her first chemo treatment for colon cancer, following surgery for removal of an intestinal tumor. She’s feeling anxious about side-effects, and has a number of questions for me about how I’ve handled my chemo treatments. I’m glad to share my experiences with her, but I have to remind her a couple of times that she’s getting completely different medications from what I’m getting, at a different frequency, and for a different total length of treatment. I encourage her to speak to the oncology nurses about side effects, or to find a fellow colon-cancer survivor to ask.
I go in for the chemo at about 10:30, which lasts until about 5:30. The medicine has done its work, unclogging the porta-cath, so everything proceeds as on previous occasions. The office is evidently crowded today, so for the first time I get a roommate in my little cubicle: a retired woman who’s there for her first chemo treatment for colon cancer, following surgery for removal of an intestinal tumor. She’s feeling anxious about side-effects, and has a number of questions for me about how I’ve handled my chemo treatments. I’m glad to share my experiences with her, but I have to remind her a couple of times that she’s getting completely different medications from what I’m getting, at a different frequency, and for a different total length of treatment. I encourage her to speak to the oncology nurses about side effects, or to find a fellow colon-cancer survivor to ask.I can hear a lot of myself in her questions, though, as I think back to my first treatments. I had done quite a bit of research ahead of time, reading books and online articles – more than this woman has done, evidently – but even so, I can remember feeling the same trepidation about side effects. I trust I'm being helpful to her, directing her to sources of information that will help her, and encouraging her to be her own advocate, asking plenty of questions.
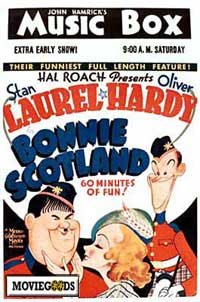 Claire drives me home, and soon after we get a lovely supper delivered by Jackie, a church member. I sample it as best I can, given the queasy feelings that are already starting. I’ve recorded an old Laurel and Hardy movie on the TiVo, Bonnie Scotland – one we’ve never seen – so we fire that up. It’s a bit of inspired nonsense that gets me through to a relatively early bedtime.
Claire drives me home, and soon after we get a lovely supper delivered by Jackie, a church member. I sample it as best I can, given the queasy feelings that are already starting. I’ve recorded an old Laurel and Hardy movie on the TiVo, Bonnie Scotland – one we’ve never seen – so we fire that up. It’s a bit of inspired nonsense that gets me through to a relatively early bedtime.Former Saturday Review editor Norman Cousins is famous for having supplemented his own medical care for chronic illness with relaxation and laughter. At one point, in consultation with his doctor, he stopped his active medical treatment, checked himself into a hotel, and filled his mind with a steady diet of humor – both books and old movies like Laurel and Hardy comedies. He says it helped him: “To the extent laughter or any of the positive emotions, can block panic, depression, or despair, we have a therapeutic ally,” he wrote later. Whatever the case, Bonnie Scotland is a good diversion.
Five treatments down, one to go.
No comments:
Post a Comment