This morning I return a voice-mail message from Dr. Lerner that I discovered late last night. The message said he'd spoken with Dr. Portlock, and wanted to touch base with me prior to my trip to New York. His answering service tracks him down, and we speak a few minutes later.
Dr. Portlock, it seems, is especially keen to see my pathology slides. After reviewing the narrative report of the PET scan indicating the size of the mass in my abdomen, she wants to have her pathologist review the slides to make sure Dr. Lerner's diagnosis is correct. She wants to confirm that it is indeed the "matted mass of enlarged lymph nodes" Dr. Lerner has supposed it to be, and not a "bulky tumor." A bulky tumor, Dr. Lerner explains, would mean a more aggressive cancer. The way to determine the true identity of the abdominal mass is by carefully analyzing the microscope slides: if the tissue sample is composed of mostly small cells, he says, I do indeed have an indolent cancer. If there are other sorts of cells there, I could be in for a very different sort of ride.
After hanging up, I begin to worry a bit. Does Dr. Portlock, the famous lymphoma specialist, have some sort of inside track that leads her to suspect I may have a more serious condition? But wait, I say to myself. She hasn't seen all the data yet: she's just responding to the narrative report from the radiologist who read the PET scan. She hasn't even seen the PET scan films. They're still inside that big envelope sitting in the entry hall of our home, awaiting my trip to New York on Tuesday.
Dr. Portlock is simply doing what a good physician does, in preparing to issue a second opinion: she's taking everything back to the beginning, so she can look at all the evidence afresh. It's entirely possible, even likely, that her diagnosis will end up being the same as Dr. Lerner's.
I'm aware of how many of Dr. Lerner's conclusions are not based on his work alone. He's the oncologist coordinating my care, but he's depending heavily on the efforts of other professionals: the technicians who have administered my various tests and scans, as well as the other physicians – radiologists and pathologists – who have read the results. I've been hearing about the importance of a team approach in treating cancer, and it seems I've already got such a team. It's just that I've just never met most of them.
All these anonymous, white-coated professionals are interested in the "mass" inside me. What a nondescript word that is! Intentionally so, at this stage of the game. It may be a collection of swollen lymph nodes, it may be a tumor, or it may be something else altogether. The word "mass" is a sort of place-holder, a temporary term for everyone to use while the diagnosis and staging of my disease is still under way. We could just as well call it a "thing," a "lump," or even a "whatchamacallit" – though none of these terms offers the proper aura of scientific objectivity.
Suddenly my situation seems rather uncertain, still – nearly three months after that day when the ultrasound technician first remarked that something on the computer monitor didn't look right. These things take time, I have to remind myself. Indeed they do...
Since my December 2, 2005 Non-Hodgkin Lymphoma diagnosis, I've been on a slow-motion journey of survivorship. Chemo wiped out my aggressive disease in May, 2006, but an indolent variety is still lurking. I had my thyroid removed due to papillary thyroid cancer in 2011, and was diagnosed with recurrent thyroid cancer in 2017. Join me for a survivor's reflections on life, death, faith, politics, the Bible and everything else. DISCLAIMER: I’m not a doctor, so don't look here for medical advice.
Saturday, December 31, 2005
December 30, 2005 - A Not-So-Long Wait, After All
Today I receive a surprise phone call from Dr. Portlock's receptionist at Memorial Sloan-Kettering Cancer Center. The doctor – who has evidently conferred with Dr. Lerner by telephone – has had a cancellation in her schedule, and is wondering if I can come see her this Tuesday, January 3rd, instead of the 17th. Of course I agree. This appointment is the most important thing on my calendar, and I'm eager to see it happen sooner, rather than later.
Just yesterday I received, in a UPS courier envelope, the pre-appointment information packet from Dr. Portlock's office – along with a lengthy list of reports, scan films and pathology tissue samples that must be faxed or shipped to New York City. There was also a stern warning that, if all these requested reports and materials were not forthcoming, my appointment would be subject to cancellation. (They don't mess around, those Sloan-Kettering people.)
I spent most of yesterday afternoon authorizing the release of these records - as well as the Fedex shipping of the films and tissue samples - so as to arrive in time for the people at Sloan-Kettering to study them prior to the 17th. Now it appears that having these items in advance is not so important as all that: with the New Year's holiday weekend looming between now and my rescheduled appointment on Tuesday, I'm supposed to simply bring them with me. (Dr. Portlock has already received the narrative reports of these tests, which Dr. Lerner's office faxed to her yesterday; it's the actual films and slides I'll bring with me that day.)
After some quick phone calls to Ocean Medical Center, the Fedex shipment of radiology and nuclear medicine films is cancelled in the nick of time, and the Pathology Department locates and packs up the biopsy slides. I pick them up from the two different offices: several very large envelopes containing the radiology and nuclear medicine films, and a small, padded mailing envelope with the tissue samples inside.
How many fruits of my medical labors of the past month or two are concentrated in those parcels! And how difficult it would be, were they to be lost! Believe me, I will be keeping very, very close track of them.
It's an odd feeling to hold the padded envelope with the tissue samples inside. Those cells, removed from the mass in my abdomen and now pressed between glass microscope slides, were once a part of my body. Yet they are also the enemy: rebel cells that are now prisoners of war, facing interrogation. I hope they spill all their secrets.
Just yesterday I received, in a UPS courier envelope, the pre-appointment information packet from Dr. Portlock's office – along with a lengthy list of reports, scan films and pathology tissue samples that must be faxed or shipped to New York City. There was also a stern warning that, if all these requested reports and materials were not forthcoming, my appointment would be subject to cancellation. (They don't mess around, those Sloan-Kettering people.)
I spent most of yesterday afternoon authorizing the release of these records - as well as the Fedex shipping of the films and tissue samples - so as to arrive in time for the people at Sloan-Kettering to study them prior to the 17th. Now it appears that having these items in advance is not so important as all that: with the New Year's holiday weekend looming between now and my rescheduled appointment on Tuesday, I'm supposed to simply bring them with me. (Dr. Portlock has already received the narrative reports of these tests, which Dr. Lerner's office faxed to her yesterday; it's the actual films and slides I'll bring with me that day.)
After some quick phone calls to Ocean Medical Center, the Fedex shipment of radiology and nuclear medicine films is cancelled in the nick of time, and the Pathology Department locates and packs up the biopsy slides. I pick them up from the two different offices: several very large envelopes containing the radiology and nuclear medicine films, and a small, padded mailing envelope with the tissue samples inside.
How many fruits of my medical labors of the past month or two are concentrated in those parcels! And how difficult it would be, were they to be lost! Believe me, I will be keeping very, very close track of them.
It's an odd feeling to hold the padded envelope with the tissue samples inside. Those cells, removed from the mass in my abdomen and now pressed between glass microscope slides, were once a part of my body. Yet they are also the enemy: rebel cells that are now prisoners of war, facing interrogation. I hope they spill all their secrets.
Tuesday, December 27, 2005
December 27, 2005 - Cancer on My Mind
"You have a life-threatening disease that requires your IMMEDIATE attention. At this moment, there is NOTHING more important than stopping EVERYTHING else that you are doing in order to consider this." Those words come from a little book I’ve been reading, From This Moment On: A Guide for Those Recently Diagnosed with Cancer, by Arlene Cotter (Random House, 1999), p. 15.
"I’ve been aware that I’ve had cancer for every hour of every day of the eight years since my diagnosis." That’s the witness of NHL survivor Dr. Elizabeth Adler, in her book, Living With Lymphoma: A Patient’s Guide (Johns Hopkins, 2005), p. xii. (By the way, that’s the most helpful book I’ve found on lymphoma, generally. It was recommended to me by our friend Don. Written by a neurobiologist who contracted NHL herself, it’s got a powerful, one-two punch of personal testimony and very detailed medical information.)
Drop everything. Think of nothing but your disease. That’s the wake-up call for the newly diagnosed. Yet, if Dr. Adler’s experience is any guide, the diagnosis continues to be life-changing, even years later.
Perhaps Dr. Adler’s claim has a bit of hyperbole to it, or maybe I’m just different from her, but I wouldn’t say I’ve spent every waking hour thinking of the disease. This has been particularly true at Christmas, as there have been many joyful family gatherings to distract me – not to mention my pastoral responsibilities in planning for three services on Christmas Eve and one on Christmas Day. Yesterday I spent more than two hours in a movie theater, watching The Chronicles of Narnia: The Lion, the Witch and the Wardrobe with the family. I can’t say I thought about lymphoma a single time during that film, nor on the drive to and from the theater, either. It was wonderful, escapist entertainment. It would be accurate to say, though, that cancer has been at least a daily, often several-times-daily, reality in my thinking. It’s hard to get away from it.
Is this constant, almost obsessive thinking part of the disease process, or part of the healing process? There’s a whole spectrum of responses, I suppose: between obsessing over illness, on the one hand, and being appropriately engaged with the work of healing, on the other.
Everything I’ve always heard from cancer experts says the patient’s mental state is crucial. The most important thing may be not so much whether we’re thinking about our illness, but how.
"I’ve been aware that I’ve had cancer for every hour of every day of the eight years since my diagnosis." That’s the witness of NHL survivor Dr. Elizabeth Adler, in her book, Living With Lymphoma: A Patient’s Guide (Johns Hopkins, 2005), p. xii. (By the way, that’s the most helpful book I’ve found on lymphoma, generally. It was recommended to me by our friend Don. Written by a neurobiologist who contracted NHL herself, it’s got a powerful, one-two punch of personal testimony and very detailed medical information.)
Drop everything. Think of nothing but your disease. That’s the wake-up call for the newly diagnosed. Yet, if Dr. Adler’s experience is any guide, the diagnosis continues to be life-changing, even years later.
Perhaps Dr. Adler’s claim has a bit of hyperbole to it, or maybe I’m just different from her, but I wouldn’t say I’ve spent every waking hour thinking of the disease. This has been particularly true at Christmas, as there have been many joyful family gatherings to distract me – not to mention my pastoral responsibilities in planning for three services on Christmas Eve and one on Christmas Day. Yesterday I spent more than two hours in a movie theater, watching The Chronicles of Narnia: The Lion, the Witch and the Wardrobe with the family. I can’t say I thought about lymphoma a single time during that film, nor on the drive to and from the theater, either. It was wonderful, escapist entertainment. It would be accurate to say, though, that cancer has been at least a daily, often several-times-daily, reality in my thinking. It’s hard to get away from it.
Is this constant, almost obsessive thinking part of the disease process, or part of the healing process? There’s a whole spectrum of responses, I suppose: between obsessing over illness, on the one hand, and being appropriately engaged with the work of healing, on the other.
Everything I’ve always heard from cancer experts says the patient’s mental state is crucial. The most important thing may be not so much whether we’re thinking about our illness, but how.
Friday, December 23, 2005
December 23, 2005 - How Are You?
Christmas will soon be upon us. Time for some last-minute shopping.
I rummage through the bag of small items I've picked up earlier for Claire's Christmas stocking. Not enough, I say to myself, trying to visualize how many small items it will take to create the obligatory bulging look, that makes for a good stocking. And so I walk down to our seaside town's little main-street shopping district, and go in and out of a few of the shops, in search of a few more stocking-stuffers.
We've got more than our share of gift shops in this resort town, and – like most locals – I don't tend to go into them very often. But this is Christmas.
In one of the shops, the proprietor greets me by name. I recognize her right away. I performed her daughter's wedding several years ago. They're not a church-member family, and I probably haven't seen her more than once or twice since the wedding, but we always give each other a cordial greeting. She fills me in on how her daughter and son-in-law are doing, in far-off Hawaii. She has a two-year-old grandchild now, she tells me. I share her joy.
"And how are you doing?" she asks.
I pause for a moment. How do I answer? It's a question I've had to face nearly every day since my diagnosis, in casual contacts with friends and strangers alike. There was a time when I'd respond to such a question with some easy pleasantry, effortlessly greasing the wheels of social interaction. But now, life is just a bit more complicated.
Do I dump the whole load, telling her I've got cancer, and am facing major changes in my life? Or do I go for the casual, stealth approach: "I'm just fine, the kids are getting bigger, the church is doing well, I've got lymphoma – and isn't it a nice day today?" Or do I avoid the subject altogether?
This time, I opt for the third approach. I tell her I'm doing OK. Not fine, or great, or fabulous – just OK. Because I am. It's the truth, or close enough to it. I'm getting by. There are plenty of worries, but also a goodly number of joys – and I don't have to look too hard to find them, especially two days before Christmas.
I've resolved to be entirely truthful about my medical condition: no secrets. But that's not quite the same thing as "the truth, the whole truth and nothing but the truth." To ladle out a full, steaming portion of truth may be too much for some appetites.
"How are you?" is a question with a multitude of meanings. It all depends on the context. Standing behind a shopping cart in the supermarket.... Sitting in an overstuffed chair a across from a psychotherapist... Perched on the crinkly paper on the edge of a doctor's examining-table... Shaking hands with parishioners at the church door... Sinking back into the bed-pillows beside one's spouse, at the end of a long day. In each context, the question has a different meaning, and a different sort of answer is expected.
Would that we could always answer that question with total honesty and forthrightness! Although I expect that, if we did, it would not be long before we'd plunge to the ground like Icarus, the wax on our wings melted from a too-close encounter with blazing human emotion. Maybe in the coming reign of God, when the lion lies down with the lamb, and every tear will be wiped from every face. But not now. Not yet.
How am I? I'm OK. Because I am.
I rummage through the bag of small items I've picked up earlier for Claire's Christmas stocking. Not enough, I say to myself, trying to visualize how many small items it will take to create the obligatory bulging look, that makes for a good stocking. And so I walk down to our seaside town's little main-street shopping district, and go in and out of a few of the shops, in search of a few more stocking-stuffers.
We've got more than our share of gift shops in this resort town, and – like most locals – I don't tend to go into them very often. But this is Christmas.
In one of the shops, the proprietor greets me by name. I recognize her right away. I performed her daughter's wedding several years ago. They're not a church-member family, and I probably haven't seen her more than once or twice since the wedding, but we always give each other a cordial greeting. She fills me in on how her daughter and son-in-law are doing, in far-off Hawaii. She has a two-year-old grandchild now, she tells me. I share her joy.
"And how are you doing?" she asks.
I pause for a moment. How do I answer? It's a question I've had to face nearly every day since my diagnosis, in casual contacts with friends and strangers alike. There was a time when I'd respond to such a question with some easy pleasantry, effortlessly greasing the wheels of social interaction. But now, life is just a bit more complicated.
Do I dump the whole load, telling her I've got cancer, and am facing major changes in my life? Or do I go for the casual, stealth approach: "I'm just fine, the kids are getting bigger, the church is doing well, I've got lymphoma – and isn't it a nice day today?" Or do I avoid the subject altogether?
This time, I opt for the third approach. I tell her I'm doing OK. Not fine, or great, or fabulous – just OK. Because I am. It's the truth, or close enough to it. I'm getting by. There are plenty of worries, but also a goodly number of joys – and I don't have to look too hard to find them, especially two days before Christmas.
I've resolved to be entirely truthful about my medical condition: no secrets. But that's not quite the same thing as "the truth, the whole truth and nothing but the truth." To ladle out a full, steaming portion of truth may be too much for some appetites.
"How are you?" is a question with a multitude of meanings. It all depends on the context. Standing behind a shopping cart in the supermarket.... Sitting in an overstuffed chair a across from a psychotherapist... Perched on the crinkly paper on the edge of a doctor's examining-table... Shaking hands with parishioners at the church door... Sinking back into the bed-pillows beside one's spouse, at the end of a long day. In each context, the question has a different meaning, and a different sort of answer is expected.
Would that we could always answer that question with total honesty and forthrightness! Although I expect that, if we did, it would not be long before we'd plunge to the ground like Icarus, the wax on our wings melted from a too-close encounter with blazing human emotion. Maybe in the coming reign of God, when the lion lies down with the lamb, and every tear will be wiped from every face. But not now. Not yet.
How am I? I'm OK. Because I am.
December 22, 2005 - A Gift of Poetry
Today, out of the blue, I receive an e-mail from a friend I haven’t heard from for some time. Bob retired as Monmouth Presbytery’s executive presbyter several years ago, and has been living in Nova Scotia. He heard of my diagnosis, and decided to send some encouraging words.
Bob’s encouragement means a lot, because - as I’ve just learned - he has had a successful battle with cancer himself.
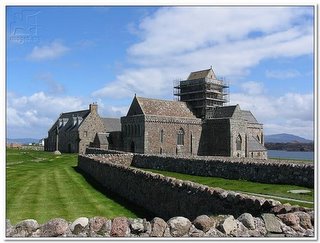 One thing Bob and I have in common is that we are both Associate Members of the Iona Community in Scotland. Here’s part of the e-mail he sent:
One thing Bob and I have in common is that we are both Associate Members of the Iona Community in Scotland. Here’s part of the e-mail he sent:
"As you have indicated, the lymphoma is in a deep, difficult place to reach - witness the (painless?) biopsy (which gave some good news). I read and re-read this prayer-poem by Maggie Wallis in the October 2005 issue of Iona Community’s Coracle. I claim that there is something else going on inside of you:
You inhabit my empty space
I watch the geese fly to you
The wind seek you endlessly
And in there
Somewhere beneath my rib cage
Is a spot I cannot touch
That aches
With the breadth and depth
Of Eternity
And that
I know is
You
All I know is that God is with us to bless and to heal. And I know God is with you NOW more than ever."
I couldn’t have said it better! Thanks, Bob.
Bob’s encouragement means a lot, because - as I’ve just learned - he has had a successful battle with cancer himself.
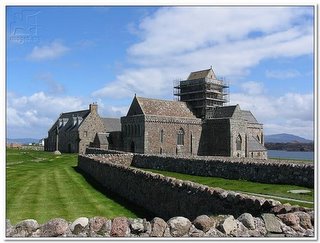 One thing Bob and I have in common is that we are both Associate Members of the Iona Community in Scotland. Here’s part of the e-mail he sent:
One thing Bob and I have in common is that we are both Associate Members of the Iona Community in Scotland. Here’s part of the e-mail he sent:"As you have indicated, the lymphoma is in a deep, difficult place to reach - witness the (painless?) biopsy (which gave some good news). I read and re-read this prayer-poem by Maggie Wallis in the October 2005 issue of Iona Community’s Coracle. I claim that there is something else going on inside of you:
You inhabit my empty space
I watch the geese fly to you
The wind seek you endlessly
And in there
Somewhere beneath my rib cage
Is a spot I cannot touch
That aches
With the breadth and depth
Of Eternity
And that
I know is
You
All I know is that God is with us to bless and to heal. And I know God is with you NOW more than ever."
I couldn’t have said it better! Thanks, Bob.
Wednesday, December 21, 2005
December 21, 2005 - When Negative is Positive
I’ve long been aware, through the course of my hospital visits as a pastor, that negative is usually positive – at least in the world of medical tests. A test that comes back negative means that the bad thing the doctors have been fearing they might find is not, in fact, there.
Such is my experience today. In the afternoon, I discover a voice mail message from Dr. Lerner’s office, asking me to please call to receive some test results. When I call back, I learn that my bone-marrow biopsy has come back negative: there’s no sign of malignancy there.
Good news, indeed! It means the cancer cells are restricted to the large mass in my abdomen and several nearby areas, and have not yet made the jump into the bone marrow (where blood cells are made). I’m still awaiting the doctor’s final assessment as to the formal staging of the disease – although he did predict, earlier, that if the bone marrow were not involved, I would likely be at stage 2. (Dr. Lerner did caution that, in follicular lymphomas like mine, the staging is not as important as the FLIPI score – which takes into account not only staging, but also several other factors that predict the success of treatment.)
Now I enter an extended waiting mode. My January 17th appointment with Dr. Portlock at Sloan-Kettering is almost a month away. My next appointment with Dr. Lerner is not until January 27th (timed to follow the assessment at Sloan-Kettering). My desire for a second opinion will end up pushing back the start of treatment by a month or more.
While a month’s delay may seem worrisome, everything I’ve learned about indolent lymphomas suggests that taking our time at this point in the process is not that big a deal. In fact, there are some very good reasons for doing so. Perhaps the most important decision related to my recovery is that of which treatment regimen to start with. Of all the decisions that must be made, this is the one to be sure to get right.
This will be a different sort of Christmas for me, and for our family. We will be more aware of the presence of darkness, of the ominous threat that has entered our lives. Yet why should we be surprised by this? Not even the first Christmas was without darkness. In the biblical story, the beatific vision of the holy child in the manger is countered by the horrors of King Herod’s jealous pursuit, and the tragic massacre of the innocents. This human life of ours is always a mix of triumph and tragedy. We take comfort where we can, remembering that "the people who walked in darkness have seen a great light" (Isaiah 9:2). Like the magi of old, we are all seekers of light.
Such is my experience today. In the afternoon, I discover a voice mail message from Dr. Lerner’s office, asking me to please call to receive some test results. When I call back, I learn that my bone-marrow biopsy has come back negative: there’s no sign of malignancy there.
Good news, indeed! It means the cancer cells are restricted to the large mass in my abdomen and several nearby areas, and have not yet made the jump into the bone marrow (where blood cells are made). I’m still awaiting the doctor’s final assessment as to the formal staging of the disease – although he did predict, earlier, that if the bone marrow were not involved, I would likely be at stage 2. (Dr. Lerner did caution that, in follicular lymphomas like mine, the staging is not as important as the FLIPI score – which takes into account not only staging, but also several other factors that predict the success of treatment.)
Now I enter an extended waiting mode. My January 17th appointment with Dr. Portlock at Sloan-Kettering is almost a month away. My next appointment with Dr. Lerner is not until January 27th (timed to follow the assessment at Sloan-Kettering). My desire for a second opinion will end up pushing back the start of treatment by a month or more.
While a month’s delay may seem worrisome, everything I’ve learned about indolent lymphomas suggests that taking our time at this point in the process is not that big a deal. In fact, there are some very good reasons for doing so. Perhaps the most important decision related to my recovery is that of which treatment regimen to start with. Of all the decisions that must be made, this is the one to be sure to get right.
This will be a different sort of Christmas for me, and for our family. We will be more aware of the presence of darkness, of the ominous threat that has entered our lives. Yet why should we be surprised by this? Not even the first Christmas was without darkness. In the biblical story, the beatific vision of the holy child in the manger is countered by the horrors of King Herod’s jealous pursuit, and the tragic massacre of the innocents. This human life of ours is always a mix of triumph and tragedy. We take comfort where we can, remembering that "the people who walked in darkness have seen a great light" (Isaiah 9:2). Like the magi of old, we are all seekers of light.
Tuesday, December 20, 2005
December 20, 2005 - In the Sloan-Kettering Book of Life
After several weeks of persistent efforts, I've finally succeeded in getting my name onto the calendar at Memorial Sloan-Kettering Cancer Center. On January 17th, I will meet with Dr. Carol Portlock, the lymphoma specialist whose name Dr. Lerner recognized when I told him about her.
It seems Dr. Portlock's office staff knows of Dr. Lerner as well. The receptionist recognized his name when I mentioned it to her. I consider that a good sign. My hope is that the two of them can collaborate on coordinating my care, and that whatever treatment regimen I may ultimately undergo can be administered in Dr. Lerner's office near our home. (I'm prepared to commute the 2+ hours to New York for chemotherapy if absolutely necessary, but I'd prefer not to – I've heard enough stories about chemo patients driving home with a nausea bucket on their knees, and would rather that drive be as short as possible.)
I've been feeling more fatigue than usual the last couple of days. I'm noticing that I'm sleeping for shorter periods of time at night, and awaking feeling more tired than usual. I've never been much of a one for midday naps – my experience has been that, even if I'm feeling tired, the best I can do is shut my eyes and doze a little, and I don't end up feeling very rested. (I can't remember much about my nursery school days, but I'd be willing to guess I was one of those kids who wiggled and squirmed through naptime!)
Is the fatigue a symptom of the lymphoma? Or is it more of a psychological response to the stress of this experience? It's hard to say, although the feelings of fatigue are unmistakable. And it feels different, somehow, from the sort of tiredness I feel when I've simply stayed up too late at night and arisen too early in the morning. My pesky internal clock seems to be getting me up at about 7:00 a.m., regardless of how tired I feel – so sleeping in doesn't seem to be an option.
Giving myself permission to stop and take a midday nap is not easy for me. My personality is closer to the "workaholic" than to the "laid-back" end of the scale. But this is probably a skill I'm going to need to learn...
It seems Dr. Portlock's office staff knows of Dr. Lerner as well. The receptionist recognized his name when I mentioned it to her. I consider that a good sign. My hope is that the two of them can collaborate on coordinating my care, and that whatever treatment regimen I may ultimately undergo can be administered in Dr. Lerner's office near our home. (I'm prepared to commute the 2+ hours to New York for chemotherapy if absolutely necessary, but I'd prefer not to – I've heard enough stories about chemo patients driving home with a nausea bucket on their knees, and would rather that drive be as short as possible.)
I've been feeling more fatigue than usual the last couple of days. I'm noticing that I'm sleeping for shorter periods of time at night, and awaking feeling more tired than usual. I've never been much of a one for midday naps – my experience has been that, even if I'm feeling tired, the best I can do is shut my eyes and doze a little, and I don't end up feeling very rested. (I can't remember much about my nursery school days, but I'd be willing to guess I was one of those kids who wiggled and squirmed through naptime!)
Is the fatigue a symptom of the lymphoma? Or is it more of a psychological response to the stress of this experience? It's hard to say, although the feelings of fatigue are unmistakable. And it feels different, somehow, from the sort of tiredness I feel when I've simply stayed up too late at night and arisen too early in the morning. My pesky internal clock seems to be getting me up at about 7:00 a.m., regardless of how tired I feel – so sleeping in doesn't seem to be an option.
Giving myself permission to stop and take a midday nap is not easy for me. My personality is closer to the "workaholic" than to the "laid-back" end of the scale. But this is probably a skill I'm going to need to learn...
Saturday, December 17, 2005
December 17, 2005 - A Passage to India
The internet is a strange and wonderful thing. I've been getting many warm, supportive comments from church friends and family who have been reading things I've written here, but one of the most remarkable is from a new friend who lives halfway around the world. Tarun Jacob is a medical doctor from India, who happened to run across my blog while doing some kind of web search. He sent me an e-mail, and we've been corresponding.
Tarun also happens to have non-Hodgkin lymphoma. He's currently receiving chemotherapy, and has a wonderful, upbeat attitude towards the whole experience. But he and I have more in common than that. First, he too has a blog, which he's been using to record his experiences; you can visit his blog by clicking here. (You really ought to check it out - he's got way more cool pictures on his blog than I do!) Second, he's a Christian. And third (along with his parents and his wife, who are also physicians), he's associated with the Christian Medical College in Vellore, India, which began as a Presbyterian medical mission and still has strong ties with the Presbyterian Church (U.S.A.). Small world!
I've written in earlier posts about what I call the Cancer Underground - that invisible network of support that has immediately reached out and enfolded me in love and caring. Well, it seems the Cancer Underground has a very long reach indeed. Amazing!
Or maybe it's not so amazing... because, I hasten to remind myself, God is at work in all of this. Who else could reach all the way to India, to arrange for a Christian brother and fellow NHL survivor to contact me and share his faith and concern?
Like I said... strange and wonderful!
Tarun also happens to have non-Hodgkin lymphoma. He's currently receiving chemotherapy, and has a wonderful, upbeat attitude towards the whole experience. But he and I have more in common than that. First, he too has a blog, which he's been using to record his experiences; you can visit his blog by clicking here. (You really ought to check it out - he's got way more cool pictures on his blog than I do!) Second, he's a Christian. And third (along with his parents and his wife, who are also physicians), he's associated with the Christian Medical College in Vellore, India, which began as a Presbyterian medical mission and still has strong ties with the Presbyterian Church (U.S.A.). Small world!
I've written in earlier posts about what I call the Cancer Underground - that invisible network of support that has immediately reached out and enfolded me in love and caring. Well, it seems the Cancer Underground has a very long reach indeed. Amazing!
Or maybe it's not so amazing... because, I hasten to remind myself, God is at work in all of this. Who else could reach all the way to India, to arrange for a Christian brother and fellow NHL survivor to contact me and share his faith and concern?
Like I said... strange and wonderful!
Thursday, December 15, 2005
December 15, 2005 - The View From the Bone-Marrow Biopsy Table
This afternoon I am lying on my left side on an examining table in Dr. Lerner’s office, while he goes about the business of conducting a bone-marrow biopsy. Earlier he has admitted that this procedure may be "a bit uncomfortable" – which I took to be a tacit admission that it’s painful.
The nurse who weighs me and leads me back to the bloodletting room seems unusually solicitous, asking very specifically how I’m feeling. I tell her I’m a bit nervous – what does she expect? – and she goes out of her way to assure me that although the procedure is uncomfortable, I will feel no pain. Not with Dr. Lerner doing it, she says, proudly.
It turns out she’s right. He’s really good. A slight prick of the needle as the doctor numbs the skin of my lower back, down near the right hip, a wait of several minutes while the anesthetic takes effect, and he goes about his work. Breathe in through your nose and out through your mouth, and do it slowly, the nurse says. She repeats the mantra several times over the next few minutes, as they’re getting me into position. Even the doctor says it at one point. I’m reminded of the Lamaze breathing exercises Claire and I practiced years ago, before the birth of our children. I find this breathing instruction both calming and anxiety-producing: calming, because that’s what that sort of breathing does; and anxiety-producing, because they’re making such a point of insisting on it.
The nurse takes her position in front of me and presses down hard on my right hip with all her weight, to immobilize me. (Not a good sign, I think to myself.) The doctor inserts his needle into the bone to draw out some fluid, telling me exactly what he’s doing at each stage of the process. I feel pressure as it goes in, but it’s not painful. Then he does the same thing with some kind of handheld device that punches into the bone as he twists it like a corkscrew. (I didn’t actually get a look at the thing, but I expect it’s one of these lovely implements: click here.) Again, I feel pressure – much greater this time – but I wouldn’t describe the sensation as pain. There’s a sort of intense throbbing, down near my tailbone, that comes and goes. Dr. Lerner remarks that my bones are stronger than those of most people for whom he does this procedure: "It’s a good thing I ate my Wheaties this morning," he quips, as he leans in harder. He says he’s used to doing bone-marrow biopsies on people much older than me, whose bones are thinner.
It’s all over in about two minutes. Dr. Lerner bandages the wound, and the nurse tells me I must lie on my back for a considerable time, with my feet flat on the table and my knees drawn up. They call Claire into the room, and we check in with Dr. Lerner on how my case is progressing.
From my awkward position on the table, I tell Dr. Lerner that, as of today, I’ve finally been assigned a doctor at Memorial Sloan-Kettering. Her name is Dr. Carol Portlock. Dr. Portlock’s office is supposed to call me very soon, to arrange an appointment. Dr. Lerner recognizes her name immediately. "She’s famous in the world of lymphoma specialists," he tells me. I tell him I’d figured as much, having Googled her name this afternoon, and discovered all manner of references to journal articles and medical-conference speeches.
I ask Dr. Lerner about my mugascan results. They came back fine, he says: no heart issues that could interfere with chemotherapy.
I ask him about staging – which rating of severity he thinks he will give to my case if the biopsy comes back positive, and which if it comes back negative (the word "staging" refers to how extensively the cancer is spread throughout the body). Dr. Lerner tells me I should not be surprised if the test comes back showing some bone marrow involvement, as this is fairly common with my type of lymphoma. Should that happen, I will be at stage 4 (the highest stage). Should the biopsy come back clean, I’ll probably be at stage 2. But don’t put too much stock in the staging numbers, he warns – because with indolent lymphomas like mine, the far more significant figure is something called the FLIPI scale ("Follicular Lymphoma Prognostic Index"). In addition to traditional staging, this scale takes into account such factors as the patient’s age, hemoglobin level, number of affected lymph nodes throughout the body, and serum LDH level (a blood-chemistry reading). The FLIPI scale is a better predictor of how patients will actually respond to treatment.
We drive back home, and I spend the next few hours sitting and resting: first in front of the television, then in the living room, as the family hangs ornaments on the Christmas tree. My role in this year’s holiday tradition is purely supervisory. When we’re finished admiring the tree and I start walking up the stairs, I experience the worst pain of the day: about the level of a really nasty pulled muscle, all up and down my right leg. I’m OK as long as I don’t walk around, so I decide to sit down at the computer and write this journal entry. It feels good to be doing something productive, after being on the receiving end of treatment all afternoon. And that, good reader, is why I’m going through this crazy exercise of keeping a cancer journal. Studying and writing about this disease and my reactions to it feels like something positive I can do. It’s a small remedy for the lack of control I’m feeling.
The nurse who weighs me and leads me back to the bloodletting room seems unusually solicitous, asking very specifically how I’m feeling. I tell her I’m a bit nervous – what does she expect? – and she goes out of her way to assure me that although the procedure is uncomfortable, I will feel no pain. Not with Dr. Lerner doing it, she says, proudly.
It turns out she’s right. He’s really good. A slight prick of the needle as the doctor numbs the skin of my lower back, down near the right hip, a wait of several minutes while the anesthetic takes effect, and he goes about his work. Breathe in through your nose and out through your mouth, and do it slowly, the nurse says. She repeats the mantra several times over the next few minutes, as they’re getting me into position. Even the doctor says it at one point. I’m reminded of the Lamaze breathing exercises Claire and I practiced years ago, before the birth of our children. I find this breathing instruction both calming and anxiety-producing: calming, because that’s what that sort of breathing does; and anxiety-producing, because they’re making such a point of insisting on it.
The nurse takes her position in front of me and presses down hard on my right hip with all her weight, to immobilize me. (Not a good sign, I think to myself.) The doctor inserts his needle into the bone to draw out some fluid, telling me exactly what he’s doing at each stage of the process. I feel pressure as it goes in, but it’s not painful. Then he does the same thing with some kind of handheld device that punches into the bone as he twists it like a corkscrew. (I didn’t actually get a look at the thing, but I expect it’s one of these lovely implements: click here.) Again, I feel pressure – much greater this time – but I wouldn’t describe the sensation as pain. There’s a sort of intense throbbing, down near my tailbone, that comes and goes. Dr. Lerner remarks that my bones are stronger than those of most people for whom he does this procedure: "It’s a good thing I ate my Wheaties this morning," he quips, as he leans in harder. He says he’s used to doing bone-marrow biopsies on people much older than me, whose bones are thinner.
It’s all over in about two minutes. Dr. Lerner bandages the wound, and the nurse tells me I must lie on my back for a considerable time, with my feet flat on the table and my knees drawn up. They call Claire into the room, and we check in with Dr. Lerner on how my case is progressing.
From my awkward position on the table, I tell Dr. Lerner that, as of today, I’ve finally been assigned a doctor at Memorial Sloan-Kettering. Her name is Dr. Carol Portlock. Dr. Portlock’s office is supposed to call me very soon, to arrange an appointment. Dr. Lerner recognizes her name immediately. "She’s famous in the world of lymphoma specialists," he tells me. I tell him I’d figured as much, having Googled her name this afternoon, and discovered all manner of references to journal articles and medical-conference speeches.
I ask Dr. Lerner about my mugascan results. They came back fine, he says: no heart issues that could interfere with chemotherapy.
I ask him about staging – which rating of severity he thinks he will give to my case if the biopsy comes back positive, and which if it comes back negative (the word "staging" refers to how extensively the cancer is spread throughout the body). Dr. Lerner tells me I should not be surprised if the test comes back showing some bone marrow involvement, as this is fairly common with my type of lymphoma. Should that happen, I will be at stage 4 (the highest stage). Should the biopsy come back clean, I’ll probably be at stage 2. But don’t put too much stock in the staging numbers, he warns – because with indolent lymphomas like mine, the far more significant figure is something called the FLIPI scale ("Follicular Lymphoma Prognostic Index"). In addition to traditional staging, this scale takes into account such factors as the patient’s age, hemoglobin level, number of affected lymph nodes throughout the body, and serum LDH level (a blood-chemistry reading). The FLIPI scale is a better predictor of how patients will actually respond to treatment.
We drive back home, and I spend the next few hours sitting and resting: first in front of the television, then in the living room, as the family hangs ornaments on the Christmas tree. My role in this year’s holiday tradition is purely supervisory. When we’re finished admiring the tree and I start walking up the stairs, I experience the worst pain of the day: about the level of a really nasty pulled muscle, all up and down my right leg. I’m OK as long as I don’t walk around, so I decide to sit down at the computer and write this journal entry. It feels good to be doing something productive, after being on the receiving end of treatment all afternoon. And that, good reader, is why I’m going through this crazy exercise of keeping a cancer journal. Studying and writing about this disease and my reactions to it feels like something positive I can do. It’s a small remedy for the lack of control I’m feeling.
December 14, 2005 - The Eye of the Needle
I have had several phone conversations in recent days with Dr. Lerner’s office staff and with staff from Sloan-Kettering, trying to resolve the question of the biopsy results, and whether I will have to undergo the procedure a second time in order to meet Sloan-Kettering’s admission requirements. Slowly the source of the problem has emerged. It appears to have been a simple misunderstanding. Something written on the narrative lab report that was faxed to Sloan-Kettering led their Lymphoma Department to think I had had only a fine-needle aspiration biopsy. I have since learned that what I actually had was both a fine-needle aspiration and a core-needle biopsy (using the largest possible needle, in fact). The Sloan-Kettering people have told Dr. Lerner’s staff that a core-needle biopsy probably did produce a large enough tissue sample for their purposes. They will know for sure when they actually receive the set of slides that was prepared by the pathologist, but they don’t anticipate a problem.
What a difference a small record-keeping glitch can make! I’m feeling relieved that a second biopsy does not appear to be in my immediate future.
Tomorrow afternoon is my bone-marrow biopsy, that procedure Dr. Lerner frankly described as "uncomfortable." I’m not looking forward to it. I’ll have to try to practice that discipline Cindy talked about, of "going to a different place."
What a difference a small record-keeping glitch can make! I’m feeling relieved that a second biopsy does not appear to be in my immediate future.
Tomorrow afternoon is my bone-marrow biopsy, that procedure Dr. Lerner frankly described as "uncomfortable." I’m not looking forward to it. I’ll have to try to practice that discipline Cindy talked about, of "going to a different place."
Monday, December 12, 2005
December 11, 2005 - Seeing You Seeing Me
Today is Sunday, a week since my announcement to the congregation. Our Chancel Choir has presented a wonderful Christmas program. I've written a narration to introduce each of the suite of familiar carols the choir is singing, and my contribution is well-received. I'm relieved that there's no need, today, to say a thing about my medical situation in worship. It's good to have a normal Sunday.
I’m aware, of course, that my health is on many church members’ minds. I wonder, now – as the people look at their pastor, do they see a person who is less than whole? If so, what difference does that make?
As I'm greeting at the door afterwards, many people bring the subject up themselves, asking how I'm feeling. It's gratifying to know how much they care. I reply that I'm feeling fine and have no symptoms. A few people who have heard the news but weren't here the previous Sunday express their concern.
I have a moment, after the greeting at the door is over, to speak with Tom and Karen, who linger at the church door. Tom has recently retired as a school administrator, and has moved into private practice as a psychological therapist. Karen is a teacher. In the past year, Karen has completed a grueling round of surgery and chemotherapy at Sloan-Kettering for breast cancer. I'm aware that one factor in Tom's decision to retire early was the experience of walking with a loved one through cancer treatment. It caused him to re-think his priorities.
Karen is looking strong and healthy. Her hair has grown back. She and Tom speak very positively about Sloan-Kettering. They tell how, in the waiting rooms, they met people who had traveled there from all over the country. With a world-class facility like that just two hours away, they reason, why go anywhere else?
It's comforting to talk with Karen and Tom. They are examples of the saying, "What does not kill me makes me stronger." The Cancer Underground strikes again.
I’m aware, of course, that my health is on many church members’ minds. I wonder, now – as the people look at their pastor, do they see a person who is less than whole? If so, what difference does that make?
As I'm greeting at the door afterwards, many people bring the subject up themselves, asking how I'm feeling. It's gratifying to know how much they care. I reply that I'm feeling fine and have no symptoms. A few people who have heard the news but weren't here the previous Sunday express their concern.
I have a moment, after the greeting at the door is over, to speak with Tom and Karen, who linger at the church door. Tom has recently retired as a school administrator, and has moved into private practice as a psychological therapist. Karen is a teacher. In the past year, Karen has completed a grueling round of surgery and chemotherapy at Sloan-Kettering for breast cancer. I'm aware that one factor in Tom's decision to retire early was the experience of walking with a loved one through cancer treatment. It caused him to re-think his priorities.
Karen is looking strong and healthy. Her hair has grown back. She and Tom speak very positively about Sloan-Kettering. They tell how, in the waiting rooms, they met people who had traveled there from all over the country. With a world-class facility like that just two hours away, they reason, why go anywhere else?
It's comforting to talk with Karen and Tom. They are examples of the saying, "What does not kill me makes me stronger." The Cancer Underground strikes again.
December 9, 2005 - Dueling Oncologists?
My first experience with administrative red tape, today, in this whole process. Certainly it will not be my last. I received a call from the admissions people at Sloan-Kettering, saying they have received copies of the test results faxed by Dr. Lerner’s office, but that these are not enough. Sloan-Kettering, it seems, will not even put me on their calendar until I can present the results of an incisional biopsy. (My previous biopsy was a fine-needle aspiration, which yields only a small quantity of tissue for pathological analysis.) An incisional biopsy is more of a surgical procedure, in which a small piece of the tumor is cut out, rather than having some liquid or semi-liquid matter sucked out through a needle.
I am sitting in a waiting area at Ocean Medical Center waiting for my mugascan. Several messages and missed connections later, I have Dr. Lerner on my cell phone. He tells me that, in his opinion, an abdominal surgical procedure is probably unnecessary, because the fine-needle biopsy has already yielded a firm diagnosis. He suggests that a core-needle biopsy, while not strictly speaking an incisional procedure, could perhaps yield enough tissue. (In a core-needle biopsy, tiny instruments are extended down the middle of a hollow needle, so small pieces of tissue may be snipped out and removed.) This could be done in the same interventional radiology suite at Ocean Medical Center where I had my fine-needle biopsy, with the same quick recovery to be expected. Of course, had we known I would be contacting Sloan-Kettering and what their requirements are, Dr. Lerner could have ordered that sort of biopsy in the first place, saving me the need to go through a second surgical procedure. But we didn’t know that; the subject of a second opinion didn’t even come up until after the diagnosis.
Dr. Lerner explains that Sloan-Kettering, being a research-oriented institution, probably has routine procedures that require a larger number of pathology slides. I wonder if there is perhaps a misunderstanding, on the part of the Sloan-Kettering people, about the location of my tumor. Many NHL patients, like Cindy, have swollen lymph nodes in easily-accessible places, just under the skin. These lumps are, for them, the first noticeable signs of the disease. My diagnosis is a bit more unusual. My tumor was detected accidentally, through an ultrasound. It’s not so easily accessible, being buried deep in my abdomen.
Back on the phone to Sloan-Kettering. The woman on the other end of the line explains that this is what "the nurse" says is needed. She has talked to him again and confirmed that, yes, this is standard policy. She offers to talk to a doctor on my behalf, but few are around the office on this particular Friday, which is the day of a major medical conference. She offers to phone me back on Monday.
I wonder at a system that gives a nurse the power to overrule an M.D. Yet maybe that’s not so surprising, in the specialized world of cancer hospitals. I’ve heard about certain oncology nurses having very deep knowledge, more than many doctors, about the narrow slice of medical knowledge that is their specialty. I silently wish Dr. Lerner could somehow speak directly with a Sloan-Kettering physician about this, and spare me the role of being the communications conduit. Yet, in fairness to him, it’s my second opinion, not his. I’ve got to do the legwork myself.
I suppose this is what the literature means when it says patients must be their own advocates. I'm learning fast about how this game is played. But it's no game. It's my life.
I am sitting in a waiting area at Ocean Medical Center waiting for my mugascan. Several messages and missed connections later, I have Dr. Lerner on my cell phone. He tells me that, in his opinion, an abdominal surgical procedure is probably unnecessary, because the fine-needle biopsy has already yielded a firm diagnosis. He suggests that a core-needle biopsy, while not strictly speaking an incisional procedure, could perhaps yield enough tissue. (In a core-needle biopsy, tiny instruments are extended down the middle of a hollow needle, so small pieces of tissue may be snipped out and removed.) This could be done in the same interventional radiology suite at Ocean Medical Center where I had my fine-needle biopsy, with the same quick recovery to be expected. Of course, had we known I would be contacting Sloan-Kettering and what their requirements are, Dr. Lerner could have ordered that sort of biopsy in the first place, saving me the need to go through a second surgical procedure. But we didn’t know that; the subject of a second opinion didn’t even come up until after the diagnosis.
Dr. Lerner explains that Sloan-Kettering, being a research-oriented institution, probably has routine procedures that require a larger number of pathology slides. I wonder if there is perhaps a misunderstanding, on the part of the Sloan-Kettering people, about the location of my tumor. Many NHL patients, like Cindy, have swollen lymph nodes in easily-accessible places, just under the skin. These lumps are, for them, the first noticeable signs of the disease. My diagnosis is a bit more unusual. My tumor was detected accidentally, through an ultrasound. It’s not so easily accessible, being buried deep in my abdomen.
Back on the phone to Sloan-Kettering. The woman on the other end of the line explains that this is what "the nurse" says is needed. She has talked to him again and confirmed that, yes, this is standard policy. She offers to talk to a doctor on my behalf, but few are around the office on this particular Friday, which is the day of a major medical conference. She offers to phone me back on Monday.
I wonder at a system that gives a nurse the power to overrule an M.D. Yet maybe that’s not so surprising, in the specialized world of cancer hospitals. I’ve heard about certain oncology nurses having very deep knowledge, more than many doctors, about the narrow slice of medical knowledge that is their specialty. I silently wish Dr. Lerner could somehow speak directly with a Sloan-Kettering physician about this, and spare me the role of being the communications conduit. Yet, in fairness to him, it’s my second opinion, not his. I’ve got to do the legwork myself.
I suppose this is what the literature means when it says patients must be their own advocates. I'm learning fast about how this game is played. But it's no game. It's my life.
December 8, 2005 - A Different Place
Another rendezvous today with a member of the Cancer Underground. Steve, pastor of a nearby Presbyterian Church, had phoned me to suggest that Claire and I meet with him and his wife Cindy, an NHL survivor. That phrase "NHL survivor" makes her sound like some grizzled, toothless ex-hockey player, when in truth Cindy is anything but. (Ah, acronyms!). We meet at the Green Planet, a local coffee shop down the street from our house.
Cindy’s NHL is similar to mine and David’s – the follicular type. She is in remission now, having received heavy doses of chemotherapy, the same CHOP-R regimen. Her first symptom was an enlarged lymph node in her neck. Surgery to remove the entire lymph node for study was easily accomplished. Cindy points out her scar: which is so inconspicuous, no one who wasn’t looking for it would ever notice.
Like David, Don and Charlotte, Cindy’s and Steve’s testimony is immensely helpful. I can’t say we leave that place feeling comforted, exactly – for she is utterly realistic about the difficult experience of chemotherapy, leading me to dread what lies ahead – but knowledge is power, and the more our knowledge increases, the more the meager power we have at our disposal likewise grows.
Cindy was living in California when she was diagnosed. She received treatment at the UCLA Medical Center. She switched to Sloan-Kettering for her follow-up care and monitoring, after she and Steve moved cross-country as he accepted the call to the church in New Jersey. She shares the name of her doctor, Paul Hamlin – one more name for my list of possible second-opinion physicians.
Cindy’s take on the chemotherapy experience is more connected with the psychology and the spirituality of it. She speaks of finding ways to "go to a different place" when the going gets tough – to be aware of the world around her, but somehow not feel so strongly connected to it. Her language calls to mind some experiences I’ve had, in places like the dentist’s chair. The last time I was at the dentist, he actually thought I was sleeping for a moment (even though the only anesthetic had been novocaine). It sounds like this is a useful skill to have, for the chemotherapy patient. I wonder if I will be able to practice this when I am lying on my stomach in Dr. Lerner’s office next Thursday for the bone-marrow biopsy, and he’s inserting a needle into my un-anesthetized pelvic bone.
At the end of our time there, the four of us pray, there in the coffee shop, holding hands. Thank God for friends – friends like Steve and Cindy, Don and Charlotte, and David – who do not wait to be called, but who simply come!
Cindy’s NHL is similar to mine and David’s – the follicular type. She is in remission now, having received heavy doses of chemotherapy, the same CHOP-R regimen. Her first symptom was an enlarged lymph node in her neck. Surgery to remove the entire lymph node for study was easily accomplished. Cindy points out her scar: which is so inconspicuous, no one who wasn’t looking for it would ever notice.
Like David, Don and Charlotte, Cindy’s and Steve’s testimony is immensely helpful. I can’t say we leave that place feeling comforted, exactly – for she is utterly realistic about the difficult experience of chemotherapy, leading me to dread what lies ahead – but knowledge is power, and the more our knowledge increases, the more the meager power we have at our disposal likewise grows.
Cindy was living in California when she was diagnosed. She received treatment at the UCLA Medical Center. She switched to Sloan-Kettering for her follow-up care and monitoring, after she and Steve moved cross-country as he accepted the call to the church in New Jersey. She shares the name of her doctor, Paul Hamlin – one more name for my list of possible second-opinion physicians.
Cindy’s take on the chemotherapy experience is more connected with the psychology and the spirituality of it. She speaks of finding ways to "go to a different place" when the going gets tough – to be aware of the world around her, but somehow not feel so strongly connected to it. Her language calls to mind some experiences I’ve had, in places like the dentist’s chair. The last time I was at the dentist, he actually thought I was sleeping for a moment (even though the only anesthetic had been novocaine). It sounds like this is a useful skill to have, for the chemotherapy patient. I wonder if I will be able to practice this when I am lying on my stomach in Dr. Lerner’s office next Thursday for the bone-marrow biopsy, and he’s inserting a needle into my un-anesthetized pelvic bone.
At the end of our time there, the four of us pray, there in the coffee shop, holding hands. Thank God for friends – friends like Steve and Cindy, Don and Charlotte, and David – who do not wait to be called, but who simply come!
December 7, 2005 - The Cancer Underground
This evening, Claire and I go to dinner at the home of Don and Charlotte, members of our church. Don is in his 70s and has NHL, of a different variety than my own. Like David, he received stem-cell replacement therapy (at Hackensack Hospital rather than Sloan-Kettering), after his chemotherapy failed to turn back the disease’s assault, and is now in remission. Don had phoned me immediately upon hearing of my diagnosis, and insisted that we come for dinner. He told me he and Charlotte had much they wanted to share with us.
We feel enfolded by warmth and caring. As David did the day before, Don also shares valuable insights about coping with the disease – and, although some of what he says parallels things David told me, it is immensely helpful for Claire to hear all of it. Charlotte describes the predictable cycles of chemotherapy, from her viewpoint as the wife of a patient: a daylong treatment, followed by a week of weakness, then a week of even more severe weakness, then finally a week of relative normality, before the whole cycle begins over again. Charlotte has a name for that third week: "Party Week," she calls it. For it is only in that week that the drugs’ declining suppression of the immune system allows for normal coming and going in public places. I have a fleeting vision of a roomful of hairless people with party hats, dancing around and sounding New Year’s noisemakers.
I wonder how closely my experience with chemo will parallel Don’s – and how that will affect my ministry at the church. So much of what I do – in leadership, in teaching, in preaching – is planned out weeks in advance. Robin and I will have to find some ways to adapt quickly to my down times during the four or five months of my treatments, especially as those down times arrive unexpectedly.
At one point, Don opens his shirt and shows us his porta-cath. It is a pronounced bump on the skin, about the size of a walnut – not the clunky plastic apparatus I had expected (the porta-caths I’ve previously seen have been of a different type, apparently). It looks more like a part of him than what I had seen before. I can see why Dr. Lerner said patients can swim with this sort of device, if they want to. Seeing the thing makes it appear less intimidating.
Sitting there with Don and Charlotte, and recalling my conversation with David of the day before, it feels almost like we’ve made contact with some sort of secret society. We’ve joined the Cancer Underground. I now have the dubious distinction of having been recommended for membership in this highly selective group. Don and Charlotte’s home feels like some kind of safe house. The information they share with us is only for the initiated. It is only when you have this disease that you are ready to hear it.
We feel enfolded by warmth and caring. As David did the day before, Don also shares valuable insights about coping with the disease – and, although some of what he says parallels things David told me, it is immensely helpful for Claire to hear all of it. Charlotte describes the predictable cycles of chemotherapy, from her viewpoint as the wife of a patient: a daylong treatment, followed by a week of weakness, then a week of even more severe weakness, then finally a week of relative normality, before the whole cycle begins over again. Charlotte has a name for that third week: "Party Week," she calls it. For it is only in that week that the drugs’ declining suppression of the immune system allows for normal coming and going in public places. I have a fleeting vision of a roomful of hairless people with party hats, dancing around and sounding New Year’s noisemakers.
I wonder how closely my experience with chemo will parallel Don’s – and how that will affect my ministry at the church. So much of what I do – in leadership, in teaching, in preaching – is planned out weeks in advance. Robin and I will have to find some ways to adapt quickly to my down times during the four or five months of my treatments, especially as those down times arrive unexpectedly.
At one point, Don opens his shirt and shows us his porta-cath. It is a pronounced bump on the skin, about the size of a walnut – not the clunky plastic apparatus I had expected (the porta-caths I’ve previously seen have been of a different type, apparently). It looks more like a part of him than what I had seen before. I can see why Dr. Lerner said patients can swim with this sort of device, if they want to. Seeing the thing makes it appear less intimidating.
Sitting there with Don and Charlotte, and recalling my conversation with David of the day before, it feels almost like we’ve made contact with some sort of secret society. We’ve joined the Cancer Underground. I now have the dubious distinction of having been recommended for membership in this highly selective group. Don and Charlotte’s home feels like some kind of safe house. The information they share with us is only for the initiated. It is only when you have this disease that you are ready to hear it.
December 6, 2005 - Help From David
Today the networking begins in earnest. I spend an hour and half visiting with David, pastor of a nearby Presbyterian Church. David is about the same age as me, and is himself an NHL survivor, now three years into remission. Like me, he has the follicular form of the disease – although he also had one of the more aggressive varieties in addition to it (it’s uncommon for one person to have more than one type, he tells me).
David was very seriously ill indeed, several years ago. He almost died, and was saved at the eleventh hour by stem-cell replacement therapy at Sloan-Kettering. I hang on his every word, for his experience is the closest thing I have seen to a road map of what’s ahead (I hope the herculean effort of stem-cell replacement will not be part of my journey, although it could be). David is particularly helpful in sketching out the various side effects of chemotherapy. He had the same "CHOP-R" (the CHOP chemotherapy cocktail, plus Rituxan) that Dr. Lerner is recommending for me.
In theological debates in presbytery meetings, David and I have not always found ourselves on the same side of the aisle. On many of the more controversial issues that divide our denomination, he is a conservative, and I am a liberal. But that matters little now. We are in this together.
In a prior telephone conversation, I had told David of my diagnosis and of my interest in going to Memorial Sloan-Kettering for a second opinion. He has already put a call in to his personal physician, Dr. Craig Moskowitz, who is on the staff of that hospital. I appreciate this most of all, and tell him so.
I leave more hopeful than when I arrived.
David was very seriously ill indeed, several years ago. He almost died, and was saved at the eleventh hour by stem-cell replacement therapy at Sloan-Kettering. I hang on his every word, for his experience is the closest thing I have seen to a road map of what’s ahead (I hope the herculean effort of stem-cell replacement will not be part of my journey, although it could be). David is particularly helpful in sketching out the various side effects of chemotherapy. He had the same "CHOP-R" (the CHOP chemotherapy cocktail, plus Rituxan) that Dr. Lerner is recommending for me.
In theological debates in presbytery meetings, David and I have not always found ourselves on the same side of the aisle. On many of the more controversial issues that divide our denomination, he is a conservative, and I am a liberal. But that matters little now. We are in this together.
In a prior telephone conversation, I had told David of my diagnosis and of my interest in going to Memorial Sloan-Kettering for a second opinion. He has already put a call in to his personal physician, Dr. Craig Moskowitz, who is on the staff of that hospital. I appreciate this most of all, and tell him so.
I leave more hopeful than when I arrived.
December 5, 2005 - Numbering the Days
Mondays are usually my day off, but today I have a funeral to conduct, in a local funeral home. The service is for a man my own age, a former member of our church, who died of chronic liver problems. His wedding had been the second one I’d performed here in this church, fifteen years ago. I had visited him in recent days in intensive care.
I go through the motions of the funeral liturgy. I imagine I’m doing an adequate job – although inside me there is an odd feeling, an awareness that everything is different now.
The timeworn words of the liturgy and of the scripture passages take on a whole new poignancy for me, even as I speak them. As Psalm 90:12 puts it, I am now "numbering my days," in a way I never have before. Will I gain "a wise heart," as a result?
After the service, the father of the deceased thanks me, and expresses particular appreciation for my being there, in light of the news I’d just received. I had made no mention of my personal health situation during the funeral service, and he had not been in our church the day before, when I'd made my announcement. How had he known? News travels fast in a small town.
I go through the motions of the funeral liturgy. I imagine I’m doing an adequate job – although inside me there is an odd feeling, an awareness that everything is different now.
The timeworn words of the liturgy and of the scripture passages take on a whole new poignancy for me, even as I speak them. As Psalm 90:12 puts it, I am now "numbering my days," in a way I never have before. Will I gain "a wise heart," as a result?
After the service, the father of the deceased thanks me, and expresses particular appreciation for my being there, in light of the news I’d just received. I had made no mention of my personal health situation during the funeral service, and he had not been in our church the day before, when I'd made my announcement. How had he known? News travels fast in a small town.
December 4, 2005 - Telling the Church
The plan I had pre-arranged with Bill swings into action. At 8 a.m. I convene our special Session meeting. Bill has offered to be there, and his presence at the table – especially at that early hour – communicates that something important is afoot.
I come right out and tell the Session members, in much the same way as I did for our kids. They express a wide range of emotions: love, concern, support, anger, dismay. They promise to be there for me, to do what needs to be done. There are times when I’ve seen the Church of Jesus Christ at its best, and this is one of those times. After a while, I leave the meeting and ask Robin to take over the moderatorial duties, so the Session members can ask Bill any questions they need to ask, without me present. I know he’s prepared to share some necessary information, about matters such as the disability provisions of the Presbyterian Pension and Benefits Plan. Who knows if it will come to that? But I would prefer not to be there, as that subject comes up.
During the announcements preceding each of the two worship services, I drop my bombshell. This is more emotional than the Session meeting – it’s worship, after all, that time when God’s people gather. This is among the hardest of things I’ve ever had to do in a worship service, and I expect my discomfort comes across in my tone of voice, my whole presentation. I explain briefly what the disease is all about, and speak of the likelihood of chemotherapy, and the associated down-time that goes along with it. There is so much we just don’t know, I tell the congregation, about what this will all mean for me, and for them. Bill leads the people in a special prayer of intercession.
Fortunately, I’ve had the foresight to ask Robin to preach on this Sunday (one small advantage of the lengthy diagnosis process is that I could pretty well predict when the shoe was going to drop). I don’t think I could have preached today. I assist with the service, but let Robin do most of the big things. As I sit up there, facing the people, I feel more self-conscious than usual. What are they thinking as they look back at me, I wonder? Will they look on me differently from now on – as a sick man, even as a dying man? Suddenly, life is so very different.
Greeting church members at the church door following the service, I experience an outpouring of support. So many people share their love and good wishes. At least a dozen people offer to drive me to medical appointments (a need I had mentioned in passing, when I made my announcement). The body of Christ does what it does best.
I come right out and tell the Session members, in much the same way as I did for our kids. They express a wide range of emotions: love, concern, support, anger, dismay. They promise to be there for me, to do what needs to be done. There are times when I’ve seen the Church of Jesus Christ at its best, and this is one of those times. After a while, I leave the meeting and ask Robin to take over the moderatorial duties, so the Session members can ask Bill any questions they need to ask, without me present. I know he’s prepared to share some necessary information, about matters such as the disability provisions of the Presbyterian Pension and Benefits Plan. Who knows if it will come to that? But I would prefer not to be there, as that subject comes up.
During the announcements preceding each of the two worship services, I drop my bombshell. This is more emotional than the Session meeting – it’s worship, after all, that time when God’s people gather. This is among the hardest of things I’ve ever had to do in a worship service, and I expect my discomfort comes across in my tone of voice, my whole presentation. I explain briefly what the disease is all about, and speak of the likelihood of chemotherapy, and the associated down-time that goes along with it. There is so much we just don’t know, I tell the congregation, about what this will all mean for me, and for them. Bill leads the people in a special prayer of intercession.
Fortunately, I’ve had the foresight to ask Robin to preach on this Sunday (one small advantage of the lengthy diagnosis process is that I could pretty well predict when the shoe was going to drop). I don’t think I could have preached today. I assist with the service, but let Robin do most of the big things. As I sit up there, facing the people, I feel more self-conscious than usual. What are they thinking as they look back at me, I wonder? Will they look on me differently from now on – as a sick man, even as a dying man? Suddenly, life is so very different.
Greeting church members at the church door following the service, I experience an outpouring of support. So many people share their love and good wishes. At least a dozen people offer to drive me to medical appointments (a need I had mentioned in passing, when I made my announcement). The body of Christ does what it does best.
December 3, 2005 - Telling Family
I call my mother in the morning. She acts as shocked as Jim and Dave did. The news is so big, she seems to have a hard time taking in all the details. Sensing denial – that predictable side-effect of life-shaking experiences – I carefully repeat several key points. After the call, I send her an e-mail putting some of the facts into writing, including also some links to a few medical web pages. It is, indeed, a lot to take in all at once.
Claire calls a couple of her sisters, and asks them to spread the word to the rest of the family. She tells her sister Eva, and also Eva’s kids, Cory and Elizabeth. I phone my cousin Eric, and ask him to tell his side of the family.
I phone Min, our church’s Clerk of Session (the Session is the local church’s governing board in the Presbyterian system). I tell her my news, and tell her I’m calling a special Session meeting for the next morning. I ask her to phone her fellow Elders – asking her not to state the reason for the meeting, just to say it’s important. (This is something I prefer to tell the Session members myself.)
There is no game plan for how to do this sort of thing. Our denominational constitution, the Book of Order, offers no help for such a fundamentally disordered situation. Were I accepting a call to another church, there are well-thought-out procedures to follow. But for a pastor trying to figure out how to tell the church’s elected leadership about a newly-diagnosed, life-threatening illness, there is no guidance. Common sense is the only guide.
I phone Lynn, our church’s Personnel Committee chair, a psychological counselor by profession. She expresses shock and grief, and offers emotional support. She marvels at the way I am delivering this information so dispassionately. I second-guess myself, after concluding the conversation with her. How am I dealing with this, after all? Am I adequately in touch with my feelings? In making all these calls, in fulfilling my responsibilities as pastor and moderator of the Session, am I merely covering up my pain with a veneer of task-oriented competence?
No, I conclude. I’m having a hard enough time with this, but I’m simply enacting a plan I’d worked out ahead of time, in consultation with Bill, our executive presbyter. Lynn and others are hearing this news for the first time; I’ve had several weeks to come to terms with it.
With all the chaos swirling around, I’m holding onto my role as pastor like a life raft. In the face of an out-of-control situation, there’s some comfort in trying to exercise control in at least one area of life. Keep a cool head. Be a non-anxious presence. Do what needs to be done. I’ve always been good at that sort of thing, when it comes to the crises of others. Now, I muse to myself, I seem to be doing the same in the midst of my own crisis. What choice do I have, anyway?
The circle of knowledge is growing ever larger.
Claire calls a couple of her sisters, and asks them to spread the word to the rest of the family. She tells her sister Eva, and also Eva’s kids, Cory and Elizabeth. I phone my cousin Eric, and ask him to tell his side of the family.
I phone Min, our church’s Clerk of Session (the Session is the local church’s governing board in the Presbyterian system). I tell her my news, and tell her I’m calling a special Session meeting for the next morning. I ask her to phone her fellow Elders – asking her not to state the reason for the meeting, just to say it’s important. (This is something I prefer to tell the Session members myself.)
There is no game plan for how to do this sort of thing. Our denominational constitution, the Book of Order, offers no help for such a fundamentally disordered situation. Were I accepting a call to another church, there are well-thought-out procedures to follow. But for a pastor trying to figure out how to tell the church’s elected leadership about a newly-diagnosed, life-threatening illness, there is no guidance. Common sense is the only guide.
I phone Lynn, our church’s Personnel Committee chair, a psychological counselor by profession. She expresses shock and grief, and offers emotional support. She marvels at the way I am delivering this information so dispassionately. I second-guess myself, after concluding the conversation with her. How am I dealing with this, after all? Am I adequately in touch with my feelings? In making all these calls, in fulfilling my responsibilities as pastor and moderator of the Session, am I merely covering up my pain with a veneer of task-oriented competence?
No, I conclude. I’m having a hard enough time with this, but I’m simply enacting a plan I’d worked out ahead of time, in consultation with Bill, our executive presbyter. Lynn and others are hearing this news for the first time; I’ve had several weeks to come to terms with it.
With all the chaos swirling around, I’m holding onto my role as pastor like a life raft. In the face of an out-of-control situation, there’s some comfort in trying to exercise control in at least one area of life. Keep a cool head. Be a non-anxious presence. Do what needs to be done. I’ve always been good at that sort of thing, when it comes to the crises of others. Now, I muse to myself, I seem to be doing the same in the midst of my own crisis. What choice do I have, anyway?
The circle of knowledge is growing ever larger.
December 2, 2005 - Diagnosis
Today, nearly a month after the first appointment with Dr. Lerner, Claire and I are again sitting in his waiting room. I am feeling less fear today, than a sort of focused intensity. It is almost a feeling of relief. The waiting is nearly over. This will surely be the day – the day we find out for sure.
I am called out of the waiting room first, to undergo the ritual bloodletting. I understand, from some of the patient memoirs I have read, that the drawing of blood is the routine first step before each consultation with the oncologist. I submit to the needle, and am thankful to feel little pain. I have years of experience as a blood donor, not to mention routine diagnostic blood tests for Dr. Cheli’s annual checkups). If the diagnosis is indeed cancer – as we’ve been reluctantly assuming it will be, based on what Dr. Lerner told us at the last visit – these blood draws will become second nature to me.
I go from the bloodletting room into an examining room, and Claire is called in to meet me there. Moments later, a nurse hands me a sheet of paper with my blood work results. Dr. Lerner and his partners have wonderful, high-tech equipment in their office that renders nearly instantaneous results – no waiting, for a hematologist’s patients. Looking the paper over, Claire and I can identify only a few of the abbreviations: "Hgb" for hemoglobin, "WBC" for white blood-cell count, "Plt" for platelets. The rest could just as well be hieroglyphics to us. We have no way of knowing whether the numbers associated with these abbreviations are within normal ranges.
It’s ironic that am holding in my hands this sheet of paper that contains the most intimate details of the inner workings of my body, but I haven’t the slightest idea what it says. These medical professionals in the office, who know so little of the inner workings of my heart in the spiritual sense, know far more than I do about the functioning of the heart muscle, and the blood it continually pumps throughout my body.
When Dr. Lerner comes in, he is as clear and matter-of-fact in his presentation as the last time. While the news he tells us is not said without kindness, it is hard news – probably the hardest news doctors must ever tell their patients.
Yes, he confirms, it is cancer. Non-Hodkins Lymphoma, of the B-cell variety. Follicular center cell. Such terms make little sense to me, but I scribble furiously on the pad I’ve brought with me for just this purpose. I’m aware that Claire is quietly crying beside me, but I continue to write, asking questions to clarify. I remember thinking to myself that maybe I ought to be crying too – for, after all, I’m the patient. But no. I am too busy to cry. These words Dr. Lerner is saying are important, and I need to record them (even though I barely understand their meaning). I know I will be surfing the Internet’s medical district that evening, to research the full implications of what the good doctor is saying.
My cancer is indolent, or slow-moving. "Indolent" means lazy. This foe of mine is lazy, lackadaisical, a true deadbeat of the cancer world. I confirm with Dr. Lerner something I have earlier read on one of those websites: that while the aggressive forms of NHL may be more immediately dangerous, they can often be cured; but that the indolent forms are basically incurable, and can only be put into remission. Yes, that is correct, Dr. Lerner assures me, in even tones. My disease is incurable. But the remissions are often long, he tells me, many years in duration. There is every reason to expect that, with treatment, I can have a great many good years ahead.
The conversation continues to unfold. We move on to the subject of treatment. "Let’s get you through the holidays," Dr. Lerner is saying. "We can begin chemotherapy in mid-January." He describes the type of chemo I will be receiving: a tripleheader cocktail known by the acronym of CHOP (three chemotherapy medicines, plus prednisone). Along with it will be Rituxan – a name I recognize from my medical webcrawling. Rituxan is a modern wonder, a genetically-engineered antibody treatment that goes directly after the particular form of cancer cells I have. It’s good news, he says, that I have this particular type of cancer, because Rituxan plus chemotherapy is a potent combination, bringing about remission in a large percentage of patients.
I will be getting a porta-cath, he tells me. I know what those are. I’ve seen them in patients I’ve visited. It’s an artificial device, implanted in the skin up near the collarbone, allowing medication to be mainlined into a major artery. Porta-caths are a kindness to patients who must receive repeated IV drips. They keep the arms from being battered and bruised by needle punctures, and they help patients avoid the burning sensation that’s a side-effect of some chemotherapy drugs. Dr. Lerner assures me that I can go around with this thing implanted in my body, and continue with all my normal activities. With this latest variety of porta-cath, he tells me, I could even go swimming if I want to (I find this hard to imagine, based on other such devices I have seen, but maybe this one is somehow different).
I’ve been wondering about how to bring up the subject of a second opinion, but Dr. Lerner does it for me. A second opinion is a good thing, he tells us. (I’m glad he brought it up, for this could be a matter of some delicacy – I’d been wondering if he’d conclude that we don’t trust him. But no, he reassures me – saying "two heads are better than one" when it comes to cancer treatment decisions.) I tell him that, yes, I would like to get a second opinion concerning treatment, and then I ask him for some recommendations. Rather than giving me specific doctors’ names, Dr. Lerner mentions the major cancer centers round about: Fox Chase in Philadelphia, New Jersey Cancer Institute in New Brunswick, Hackensack Hospital – and in New York City, Memorial Sloan-Kettering and Cornell. It’s quite a list, reflecting the embarrassment of riches we have in this area for treatment of this disease. He gives no further recommendation, saying it’s my choice which one – if any – to contact.
I sense that this is a rule of the game. This is as far as he’ll go, and no further. The next step is up to us. Dr. Lerner will be happy to work with a second-opinion doctor, but it’s up to us to find such a person.
Fair enough. We can do that. But how do we decide where to go? And, more to the point, what do we do if the second-opinion doctor disagrees with Dr. Lerner as to the course of treatment? How on earth do we, lacking a medical-school education, decide between a couple of dueling oncologists? That’s a question for another day, and one I hope we will never have to deal with. But I do know I want that second opinion, and tell Dr. Lerner so.
More tests are ahead, he tells us: first, a mugascan (a sort of x-ray of the heart, to make sure there are no abnormalities that could interfere with chemotherapy). And then – the news I have been vaguely dreading – a bone-marrow biopsy. I’ve heard about those, about how uncomfortable they can be. I press Dr. Lerner for some details. He refuses to sugar-coat it: this test is uncomfortable (he stops short of using the word "pain," I notice). He says can numb the surface of the skin with novocaine, but there’s no way he can numb the underlying bone. He will perform the procedure himself, right in the office. He’ll make it quick. Well, "quick" is some small comfort, I suppose.
The mugascan prescription is duly inscribed, the bone-marrow biopsy appointment duly made, and we make our way back out into the waiting room. Sitting there, as we exit, is Cindy, a member of our church. She informs us she’s brought her eighteen-year-old daughter to see one of the doctors in the group (I’d visited her daughter a couple weeks before in the hospital, as she was being treated for a mysterious, low-platelet-level blood problem).
And what am I doing here, she asks, with a tone of concern? Here we go. This is the first person we have to tell.
I’ve just received life-changing news, I inform her. I’ve been diagnosed with lymphoma.
I’m so sorry, says Cindy. Yes, I say, so am I. Life is going to be very different. We thank her for her concern, wish her daughter well, then pull on our coats and leave the building.
On the way out to the car, Claire asks whether I was sure I did the right thing in telling Cindy the news. It’s Friday, I say to her. Tonight we tell the kids, and after that we start phoning relatives. On Sunday, we tell the whole congregation, and after that the whole world can know. It really doesn’t matter now. I’ve resolved to be very open about my condition, I remind her. No more secrets. There’s something oddly liberating in that.
We sit together in the car for a few minutes, holding hands. I tell Claire I’ve been feeling very close to her through this ordeal. I thank her for being there for me. We confess to one another how frightened we both feel. But there is love there, too – more love than I could have imagined I would feel, in such circumstances. Such love is a lantern in a dark time.
I take out my cell phone and call our son Benjamin (who’s living, this year, in a rental house with a few friends, while attending Monmouth University). Come home tonight, we tell him. We’ve got to have a family meeting. We can’t explain why. Just come. He makes a few feeble attempts to question us further on the reason for the meeting, but then he agrees. We drive home.
An hour or so later, Ben shows up. Ania is already there; she has made plans to go out with friends this evening, but we ask her to cancel. We sit at the kitchen table, and I come right out with it (what else could I do?). I’ve been diagnosed with Non-Hodgkins Lymphoma, I tell them. It is a form of cancer. It’s highly treatable, but the treatment is difficult. There is no cure, but there is the prospect of long remissions, if the treatment succeeds.
Ania sits quietly, looking like she’s seen a ghost. She has, I think to myself. The ghost is me. Ben expresses a bit more emotion, appropriately commiserating about the unfairness of it all, and asking some good, pertinent questions.
I phone Bill, our presbytery executive (he fills a position roughly comparable to that of bishop in some other denominations, but is also a sort of pastor to the pastors). Bill and I had prearranged this call. I had taken him into my confidence a couple of weeks before, so he could be prepared for the worst. I had outlined to him at the time my resolve to be completely open about this, once we had a firm diagnosis – fully informing the congregation at the earliest opportunity. He had asked me to call him, once I knew. I do so, and feel strengthened by his support and understanding.
A little later I get on the phone, and call my brothers: Jim in Boston, Dave in San Francisco. I repeat the same procedure we followed with Ben and Ania. No easy way to say this: it’s cancer, it’s treatable, etc., etc. They respnd with shock, and with expressions of support. By now it’s too late to call our mother, in her retirement community in Chapel Hill, North Carolina. Tomorrow is another day.
I am called out of the waiting room first, to undergo the ritual bloodletting. I understand, from some of the patient memoirs I have read, that the drawing of blood is the routine first step before each consultation with the oncologist. I submit to the needle, and am thankful to feel little pain. I have years of experience as a blood donor, not to mention routine diagnostic blood tests for Dr. Cheli’s annual checkups). If the diagnosis is indeed cancer – as we’ve been reluctantly assuming it will be, based on what Dr. Lerner told us at the last visit – these blood draws will become second nature to me.
I go from the bloodletting room into an examining room, and Claire is called in to meet me there. Moments later, a nurse hands me a sheet of paper with my blood work results. Dr. Lerner and his partners have wonderful, high-tech equipment in their office that renders nearly instantaneous results – no waiting, for a hematologist’s patients. Looking the paper over, Claire and I can identify only a few of the abbreviations: "Hgb" for hemoglobin, "WBC" for white blood-cell count, "Plt" for platelets. The rest could just as well be hieroglyphics to us. We have no way of knowing whether the numbers associated with these abbreviations are within normal ranges.
It’s ironic that am holding in my hands this sheet of paper that contains the most intimate details of the inner workings of my body, but I haven’t the slightest idea what it says. These medical professionals in the office, who know so little of the inner workings of my heart in the spiritual sense, know far more than I do about the functioning of the heart muscle, and the blood it continually pumps throughout my body.
When Dr. Lerner comes in, he is as clear and matter-of-fact in his presentation as the last time. While the news he tells us is not said without kindness, it is hard news – probably the hardest news doctors must ever tell their patients.
Yes, he confirms, it is cancer. Non-Hodkins Lymphoma, of the B-cell variety. Follicular center cell. Such terms make little sense to me, but I scribble furiously on the pad I’ve brought with me for just this purpose. I’m aware that Claire is quietly crying beside me, but I continue to write, asking questions to clarify. I remember thinking to myself that maybe I ought to be crying too – for, after all, I’m the patient. But no. I am too busy to cry. These words Dr. Lerner is saying are important, and I need to record them (even though I barely understand their meaning). I know I will be surfing the Internet’s medical district that evening, to research the full implications of what the good doctor is saying.
My cancer is indolent, or slow-moving. "Indolent" means lazy. This foe of mine is lazy, lackadaisical, a true deadbeat of the cancer world. I confirm with Dr. Lerner something I have earlier read on one of those websites: that while the aggressive forms of NHL may be more immediately dangerous, they can often be cured; but that the indolent forms are basically incurable, and can only be put into remission. Yes, that is correct, Dr. Lerner assures me, in even tones. My disease is incurable. But the remissions are often long, he tells me, many years in duration. There is every reason to expect that, with treatment, I can have a great many good years ahead.
The conversation continues to unfold. We move on to the subject of treatment. "Let’s get you through the holidays," Dr. Lerner is saying. "We can begin chemotherapy in mid-January." He describes the type of chemo I will be receiving: a tripleheader cocktail known by the acronym of CHOP (three chemotherapy medicines, plus prednisone). Along with it will be Rituxan – a name I recognize from my medical webcrawling. Rituxan is a modern wonder, a genetically-engineered antibody treatment that goes directly after the particular form of cancer cells I have. It’s good news, he says, that I have this particular type of cancer, because Rituxan plus chemotherapy is a potent combination, bringing about remission in a large percentage of patients.
I will be getting a porta-cath, he tells me. I know what those are. I’ve seen them in patients I’ve visited. It’s an artificial device, implanted in the skin up near the collarbone, allowing medication to be mainlined into a major artery. Porta-caths are a kindness to patients who must receive repeated IV drips. They keep the arms from being battered and bruised by needle punctures, and they help patients avoid the burning sensation that’s a side-effect of some chemotherapy drugs. Dr. Lerner assures me that I can go around with this thing implanted in my body, and continue with all my normal activities. With this latest variety of porta-cath, he tells me, I could even go swimming if I want to (I find this hard to imagine, based on other such devices I have seen, but maybe this one is somehow different).
I’ve been wondering about how to bring up the subject of a second opinion, but Dr. Lerner does it for me. A second opinion is a good thing, he tells us. (I’m glad he brought it up, for this could be a matter of some delicacy – I’d been wondering if he’d conclude that we don’t trust him. But no, he reassures me – saying "two heads are better than one" when it comes to cancer treatment decisions.) I tell him that, yes, I would like to get a second opinion concerning treatment, and then I ask him for some recommendations. Rather than giving me specific doctors’ names, Dr. Lerner mentions the major cancer centers round about: Fox Chase in Philadelphia, New Jersey Cancer Institute in New Brunswick, Hackensack Hospital – and in New York City, Memorial Sloan-Kettering and Cornell. It’s quite a list, reflecting the embarrassment of riches we have in this area for treatment of this disease. He gives no further recommendation, saying it’s my choice which one – if any – to contact.
I sense that this is a rule of the game. This is as far as he’ll go, and no further. The next step is up to us. Dr. Lerner will be happy to work with a second-opinion doctor, but it’s up to us to find such a person.
Fair enough. We can do that. But how do we decide where to go? And, more to the point, what do we do if the second-opinion doctor disagrees with Dr. Lerner as to the course of treatment? How on earth do we, lacking a medical-school education, decide between a couple of dueling oncologists? That’s a question for another day, and one I hope we will never have to deal with. But I do know I want that second opinion, and tell Dr. Lerner so.
More tests are ahead, he tells us: first, a mugascan (a sort of x-ray of the heart, to make sure there are no abnormalities that could interfere with chemotherapy). And then – the news I have been vaguely dreading – a bone-marrow biopsy. I’ve heard about those, about how uncomfortable they can be. I press Dr. Lerner for some details. He refuses to sugar-coat it: this test is uncomfortable (he stops short of using the word "pain," I notice). He says can numb the surface of the skin with novocaine, but there’s no way he can numb the underlying bone. He will perform the procedure himself, right in the office. He’ll make it quick. Well, "quick" is some small comfort, I suppose.
The mugascan prescription is duly inscribed, the bone-marrow biopsy appointment duly made, and we make our way back out into the waiting room. Sitting there, as we exit, is Cindy, a member of our church. She informs us she’s brought her eighteen-year-old daughter to see one of the doctors in the group (I’d visited her daughter a couple weeks before in the hospital, as she was being treated for a mysterious, low-platelet-level blood problem).
And what am I doing here, she asks, with a tone of concern? Here we go. This is the first person we have to tell.
I’ve just received life-changing news, I inform her. I’ve been diagnosed with lymphoma.
I’m so sorry, says Cindy. Yes, I say, so am I. Life is going to be very different. We thank her for her concern, wish her daughter well, then pull on our coats and leave the building.
On the way out to the car, Claire asks whether I was sure I did the right thing in telling Cindy the news. It’s Friday, I say to her. Tonight we tell the kids, and after that we start phoning relatives. On Sunday, we tell the whole congregation, and after that the whole world can know. It really doesn’t matter now. I’ve resolved to be very open about my condition, I remind her. No more secrets. There’s something oddly liberating in that.
We sit together in the car for a few minutes, holding hands. I tell Claire I’ve been feeling very close to her through this ordeal. I thank her for being there for me. We confess to one another how frightened we both feel. But there is love there, too – more love than I could have imagined I would feel, in such circumstances. Such love is a lantern in a dark time.
I take out my cell phone and call our son Benjamin (who’s living, this year, in a rental house with a few friends, while attending Monmouth University). Come home tonight, we tell him. We’ve got to have a family meeting. We can’t explain why. Just come. He makes a few feeble attempts to question us further on the reason for the meeting, but then he agrees. We drive home.
An hour or so later, Ben shows up. Ania is already there; she has made plans to go out with friends this evening, but we ask her to cancel. We sit at the kitchen table, and I come right out with it (what else could I do?). I’ve been diagnosed with Non-Hodgkins Lymphoma, I tell them. It is a form of cancer. It’s highly treatable, but the treatment is difficult. There is no cure, but there is the prospect of long remissions, if the treatment succeeds.
Ania sits quietly, looking like she’s seen a ghost. She has, I think to myself. The ghost is me. Ben expresses a bit more emotion, appropriately commiserating about the unfairness of it all, and asking some good, pertinent questions.
I phone Bill, our presbytery executive (he fills a position roughly comparable to that of bishop in some other denominations, but is also a sort of pastor to the pastors). Bill and I had prearranged this call. I had taken him into my confidence a couple of weeks before, so he could be prepared for the worst. I had outlined to him at the time my resolve to be completely open about this, once we had a firm diagnosis – fully informing the congregation at the earliest opportunity. He had asked me to call him, once I knew. I do so, and feel strengthened by his support and understanding.
A little later I get on the phone, and call my brothers: Jim in Boston, Dave in San Francisco. I repeat the same procedure we followed with Ben and Ania. No easy way to say this: it’s cancer, it’s treatable, etc., etc. They respnd with shock, and with expressions of support. By now it’s too late to call our mother, in her retirement community in Chapel Hill, North Carolina. Tomorrow is another day.
November 26, 2005 - An End-of-Radiation Party
We attend a party at the home of Donna, a friend, to celebrate the end of her radiation treatments for breast cancer. Previously, she had undergone chemotherapy. There she is, with her peach-fuzz hair beginning to grow back, but otherwise looking strong and healthy. There is laughter in her eyes. So there is light at the end of the chemo-and-radiation tunnel.
It is a heartening event. A houseful of people: laughing, conversing, eating, doing all the things people do at parties. A community gathering close, to enfold one of their own – one who was nearly lost, but now is found. I cannot yet speak publicly of the fears that fill me, but I can sense the power of community to heal.
It is a heartening event. A houseful of people: laughing, conversing, eating, doing all the things people do at parties. A community gathering close, to enfold one of their own – one who was nearly lost, but now is found. I cannot yet speak publicly of the fears that fill me, but I can sense the power of community to heal.
November 24, 2005 - Thanksgiving
It’s Thanksgiving Day. Claire and I have planned a smaller-than-usual gathering. This year we decided not to invite any church members, as we often do – to keep it as just a family gathering. Still, we have about fifteen around the table, including three of Claire’s siblings and their children: her sister Eva and her two kids, her brother Victor from Baltimore and his two kids, and her sister Ramona from New York. There’s also a friend of Ramona’s whom she invited at the last minute (this violates our family-only decision, but one guest we figured we could handle).
I cooked the turkey as usual, along with its stuffing and gravy, and Claire took care of the other dishes, with help from various family members. In these days when I have been experiencing lower energy levels than usual, I find myself wondering whether this is due to my physical condition, or to depression.
As we sit down at the table for our usual Thanksgiving grace – a task which (for some reason I’ve never figured out) falls to me, even though Claire is also a minister – Claire suggests a new procedure. Each person, she announces, will think of the person to the left, and then say one thing he or she appreciates about that person. I’m sitting to the left of Victor, a proverbial "man of few words." He says he’s thankful that I’ve always been there for members of the Pula family, in times of difficulty. He calls me "the rock."
Little does he know...
I cooked the turkey as usual, along with its stuffing and gravy, and Claire took care of the other dishes, with help from various family members. In these days when I have been experiencing lower energy levels than usual, I find myself wondering whether this is due to my physical condition, or to depression.
As we sit down at the table for our usual Thanksgiving grace – a task which (for some reason I’ve never figured out) falls to me, even though Claire is also a minister – Claire suggests a new procedure. Each person, she announces, will think of the person to the left, and then say one thing he or she appreciates about that person. I’m sitting to the left of Victor, a proverbial "man of few words." He says he’s thankful that I’ve always been there for members of the Pula family, in times of difficulty. He calls me "the rock."
Little does he know...
November 23, 2005 - Things to Come
Today I am reading Dancing At the Edge of Life, a 1998 memoir by a lymphoma patient named Gale Warner. Her story, like mine, also began with an unexplained mass inside her torso – although in her case, it was located up near the shoulder blade, rather than in the abdomen. She eventually died from her disease.
I find Gale's story to be of compelling interest – particularly her graphic descriptions of chemotherapy and its side effects. I keep telling myself, as I read, that Gale underwent her chemotherapy treatments in the mid-1990s – eons ago, in the rapidly-developing cancer-treatment field. Yet I expect that many of the side-effects are still the same. I particularly remember her descriptions of how many hours it takes to receive chemo, and how fatigue and mental fogginess are common side-effects. Chemotherapy, she says, crowds out nearly everything else in life, during those long hours of sitting in a recliner in the treatment center, while poison drips into the veins.
Given my rapidly-emerging, existential interest in this subject – even at this early stage, before my diagnosis is even confirmed – I can relate to her perspective.
Chemotherapy. Is there any way to get ready for it?
I find Gale's story to be of compelling interest – particularly her graphic descriptions of chemotherapy and its side effects. I keep telling myself, as I read, that Gale underwent her chemotherapy treatments in the mid-1990s – eons ago, in the rapidly-developing cancer-treatment field. Yet I expect that many of the side-effects are still the same. I particularly remember her descriptions of how many hours it takes to receive chemo, and how fatigue and mental fogginess are common side-effects. Chemotherapy, she says, crowds out nearly everything else in life, during those long hours of sitting in a recliner in the treatment center, while poison drips into the veins.
Given my rapidly-emerging, existential interest in this subject – even at this early stage, before my diagnosis is even confirmed – I can relate to her perspective.
Chemotherapy. Is there any way to get ready for it?
November 22, 2005 - Biopsy
Claire and I arise before dawn and drive the five miles or so to Ocean Medical Center. Our sixteen-year-old daughter Ania had been curious, the evening before, about why I had to go to the hospital. Claire told her it was just a medical procedure. (Technically true, but still far less than the truth.) But we’re agreed that now is not yet the time to tell her. Thankfully, she didn’t ask for any further information.
At the hospital, I end up in the new interventional radiology suite. When I make my way back into the outpatient-procedure staging area, I find that my nurse is none other than Tom, an active member of our church who frequently ushers on Sunday mornings. I’ve always respected Tom’s professionalism as a nurse, as I’ve seen him at work in the course of my hospital rounds, and my good impression is confirmed today. He is appropriately concerned, and responds with genuine sympathy when I tell him of the possible lymphoma diagnosis. He assures me he will keep my situation confidential, and I trust him.
From my vantage-point lying on the gurney, I can see two other people I know: Diantha, another member of our church – a longtime hospital volunteer who works in this unit – and Charlie, member of a nearby Presbyterian church and the grandfather of two of our church members. There’s no anonymity in a small town, I remind myself. Neither one comes over to speak with me, though, for which I’m thankful. I’d rather keep the circle small. (Claire will tell me later on that she spoke with Diantha, but that she had discreetly asked no questions about the reason I was there.)
After being wheeled into the little anteroom outside the interventional radiology suite, I discover that the nurse there also knows me. She happens to be the sister-in-law of a church member, and remembers me from when I conducted a funeral for a family member a year before. I mention my desire for confidentiality, and hope for the best.
The staff inside the high-tech procedure room is cheery and professional. They administer what they jokingly refer to as "happy juice," through an IV line. My recollections from that point on are dim. I recall the nurses talking to me, and one of them shaving the hair from my abdomen and swabbing it with disinfectant, but I have little recollection of what follows – although I do recall Dr. Feng, the radiologist, telling me some time later that he’s about to take the tissue sample, and hear a clicking sound as he does so. Somehow, the medicine will blot out all other memories. The CIA could use this stuff for brainwashing.
The nurse who spoke with me in the anteroom told me all about how wonderful this medication feels, and how patients frequently ask if they can have some more, but that’s not my experience. "Happy juice," they call it? No happiness for me – just blessed indifference. But it accomplishes its purpose well enough. I awaken back in the outpatient-surgery staging area, with the comforting sight of Tom hovering around and Claire sitting by my side. I recover quickly, and we return home. I nap for a couple of hours, then walk over to the church late in the afternoon. The day before, I had told Diane, our church secretary, that I would be taking the morning off for a medical test, but today she asks for no further details. The soul of discretion, is Diane.
At the hospital, I end up in the new interventional radiology suite. When I make my way back into the outpatient-procedure staging area, I find that my nurse is none other than Tom, an active member of our church who frequently ushers on Sunday mornings. I’ve always respected Tom’s professionalism as a nurse, as I’ve seen him at work in the course of my hospital rounds, and my good impression is confirmed today. He is appropriately concerned, and responds with genuine sympathy when I tell him of the possible lymphoma diagnosis. He assures me he will keep my situation confidential, and I trust him.
From my vantage-point lying on the gurney, I can see two other people I know: Diantha, another member of our church – a longtime hospital volunteer who works in this unit – and Charlie, member of a nearby Presbyterian church and the grandfather of two of our church members. There’s no anonymity in a small town, I remind myself. Neither one comes over to speak with me, though, for which I’m thankful. I’d rather keep the circle small. (Claire will tell me later on that she spoke with Diantha, but that she had discreetly asked no questions about the reason I was there.)
After being wheeled into the little anteroom outside the interventional radiology suite, I discover that the nurse there also knows me. She happens to be the sister-in-law of a church member, and remembers me from when I conducted a funeral for a family member a year before. I mention my desire for confidentiality, and hope for the best.
The staff inside the high-tech procedure room is cheery and professional. They administer what they jokingly refer to as "happy juice," through an IV line. My recollections from that point on are dim. I recall the nurses talking to me, and one of them shaving the hair from my abdomen and swabbing it with disinfectant, but I have little recollection of what follows – although I do recall Dr. Feng, the radiologist, telling me some time later that he’s about to take the tissue sample, and hear a clicking sound as he does so. Somehow, the medicine will blot out all other memories. The CIA could use this stuff for brainwashing.
The nurse who spoke with me in the anteroom told me all about how wonderful this medication feels, and how patients frequently ask if they can have some more, but that’s not my experience. "Happy juice," they call it? No happiness for me – just blessed indifference. But it accomplishes its purpose well enough. I awaken back in the outpatient-surgery staging area, with the comforting sight of Tom hovering around and Claire sitting by my side. I recover quickly, and we return home. I nap for a couple of hours, then walk over to the church late in the afternoon. The day before, I had told Diane, our church secretary, that I would be taking the morning off for a medical test, but today she asks for no further details. The soul of discretion, is Diane.
November 21, 2005 - On the Eve of the Biopsy
I find myself getting increasingly anxious about the needle biopsy, which is scheduled for tomorrow. I've read in one of the personal memoirs I checked out from the library (Stranger in the Village of the Sick, by Paul Stoller) about the author's own biopsy, which his doctor performed using only a local anesthetic. I’ve been told by the caller from the hospital who scheduled my procedure that I, too, will have only a local. I have visions of a surgical-masked doctor brandishing a huge hypodermic needle and saying in a simpering, Peter Lorre voice, "We are ready to puncture your abdomen now."
When someone else calls today to give me last-minute instructions, I ask her about the anesthetic issue. She assures me that I will be given "sedation," as well as a local anesthetic. When I press her for more details, saying the other caller told me I'd only have a local, she says that’s not correct. "We’re not vultures here. We’ll keep you comfortable."
Thank the Lord. I retire with much less anxiety about the next day.
When someone else calls today to give me last-minute instructions, I ask her about the anesthetic issue. She assures me that I will be given "sedation," as well as a local anesthetic. When I press her for more details, saying the other caller told me I'd only have a local, she says that’s not correct. "We’re not vultures here. We’ll keep you comfortable."
Thank the Lord. I retire with much less anxiety about the next day.
November 18, 2005 - Library

I take some time off this afternoon, and drive to my hometown of Toms River, to the main branch of the Ocean County Library. I could have saved time and gone to our local branch in Point Pleasant Beach, but a couple of church members work behind the circulation desk, and I don’t want it to be generally known what sort of books I’m checking out these days. It’s a small town, after all. And besides, I tell myself, the collection at the main branch is larger, anyway.
I nearly don’t make it into the library. The entrances are barricaded, and I see evident signs of construction as I look through the glass. I dimly recall having read in the paper about a major renovation project at the library’s main branch, that would close the place completely for several weeks. I start back to my car, but then rethink that decision. I reverse course and walk further around the building, just to make sure. When I do, I find that a side entrance door is unlocked, and the library is open for business after all. The library staff has done an incredibly poor job of putting up signs announcing that the place is still open.
Feeling anger boil within me, I compose myself and walk up to a woman working behind the circulation desk. There is no sign posted outside, I say to her, and doesn’t she know that patrons are probably turning around going back home, thinking the library is still closed? Please do something to make sure some kind of sign goes up, I said to her, politely but firmly – but probably with suppressed anger in my voice.
"It’s not my job," she says curtly, in response. There were some signs, she explains, but they blew away in yesterday’s high winds. I think to myself how easy it would have been for her to take a marker and a piece of paper and tape a hand-lettered sign to the inside of the glass.
"That may be," I persist, "but that doesn’t help people coming here from out of town. I drove a half hour to get here, and very nearly turned around and went home!"
"I know, it’s a problem," she admits, feebly.
"Well, please make sure a sign goes up," I say, and stride past her into the main part of the library – thinking unkind thoughts to myself about the bureaucratic mentality that leads people to hide behind lame excuses like, "It’s not my job."
Where had my anger come from? I hadn’t been feeling angry, on a conscious level, as I made my way to the library. Yet, somewhere beneath the surface, I was evidently seething at the injustice of my situation. The anger emerged, transforming me into Lancelot of the Library, righting wrongs on behalf of book-lovers everywhere.
After a quick glance at the library catalog on a computer terminal, I go upstairs and find several shelves filled with books on the subject of cancer. Easily half the titles are about breast cancer (why that variety of cancer is deemed so much more worthy of either publishers’ or acquisition librarians’ attention, I can’t say). But there are some good general books as well. Unlike the plethora of breast-cancer books, there is not one volume dedicated exclusively to lymphoma.
I am looking especially for memoirs by cancer survivors. In these days before I’m comfortable showing my face in any support groups, I’m feeling an urgent need to listen to the voices of others who have traveled this road before me.
I carry a whole stack of books to a comfortable chair in one corner of the stacks area, and begin to skim through them. With the technically-oriented volumes, I discard those with a copyright date of more than a few years ago (science is changing so rapidly, I reason, they’re probably outdated). I’m a bit more flexible when it comes to the personal memoirs. While some of the descriptions of drugs and technical procedures may be outdated, the human emotions of dealing with the disease surely aren’t.
After returning home and engaging in some testy responses with Claire over inconsequential things, it occurs to me that I’m still feeling deeply angry about all of this. Normally, I enjoy research, but there are so many other subjects I’d rather spend time looking into than this one.
November 16, 2005 - Telling Robin - and Getting a PET Scan
Today I broaden the small circle of those who know of my condition. I tell Robin. She’s recently come back to work, part-time. I haven’t wanted to tell her while she’s still in the thick of things with physical therapy, pain medications, etc., but now that she’s well enough to ease back into her ministry at the church, it seems that now is the time.
She is, of course, shocked. I find her empathy reassuring. After speaking with me, she walks across the street to the Manse, leaning on her cane, and shares a few supportive words for Claire as well.
I’m uncomfortable with all the secrets, and am looking forward to the day when – whatever the outcome of all these diagnostic procedures – we can be public about my health situation. One of the hardest things about a cancer diagnosis, I’ve always been told, is the lengthy waiting period while initial clinical intuitions are being confirmed. I’m certainly finding that to be true.
I’m reflecting back, now, on my PET scan – conducted on November 14th at Jersey Shore University Medical Center...
The PET Scan is much like a CT Scan. I must go to Jersey Shore University Medical Center for this test, because the machine is not available at Ocean Medical Center. As it turns out, it’s not even located at Jersey Shore (at least not on a permanent basis). To reach the unit, I walk down a corridor that takes me to the very edge of the building. I feel a slight draft as I walk through an odd sort of door, draped with cloth around the edges, and I realize I’ve stepped out of the building and onto a tractor-trailer truck. The PET Scanner evidently moves, on a regular schedule, among several different hospitals – so expensive is this piece of equipment, that the hospitals must share it. Once through the connecting gateway, I feels like I'm in any other windowless room in a medical facility. Soft, new-age music is playing through speakers in the ceiling.
The technician is friendly and efficient. He sits me down in a chair and administers a dose of something into my arm, intravenously. This is radioactive glucose, he tells me. I will sit there for a half-hour and wait while it makes its way through my body. The radioactive glucose will head directly to the cells in my body that have a high metabolic rate – these are the malignancies. Then, the PET scanner will be able to identify the "hot spots" that are likely to be cancer.
When the patient ahead of me is finished, the technician asks me to lie down on a sort of plastic stretcher, on my back. I am supposed to lie absolutely still. An electric motor kicks into life, sliding me smoothly, feet first, into the large, donut-shaped device that is the PET scanner. Starting near my waist, the machine moves me slowly, in intervals of five minutes or so, deeper into the scanner.
Some patients report difficulties with claustrophobia in machines like this, and I can see why. By the time I’m reaching the end of the process, my face is just inches away from the machine, which makes whirring and clicking noises. I find that closing my eyes is easier than keeping them open. The hardest part of the half-hour scan, for me, is lying face-up on the narrow plastic stretcher: in the last ten minutes or so, with my arms extended over my head. I go home, curious about the results, but knowing I will not hear for some time.
She is, of course, shocked. I find her empathy reassuring. After speaking with me, she walks across the street to the Manse, leaning on her cane, and shares a few supportive words for Claire as well.
I’m uncomfortable with all the secrets, and am looking forward to the day when – whatever the outcome of all these diagnostic procedures – we can be public about my health situation. One of the hardest things about a cancer diagnosis, I’ve always been told, is the lengthy waiting period while initial clinical intuitions are being confirmed. I’m certainly finding that to be true.
I’m reflecting back, now, on my PET scan – conducted on November 14th at Jersey Shore University Medical Center...
The PET Scan is much like a CT Scan. I must go to Jersey Shore University Medical Center for this test, because the machine is not available at Ocean Medical Center. As it turns out, it’s not even located at Jersey Shore (at least not on a permanent basis). To reach the unit, I walk down a corridor that takes me to the very edge of the building. I feel a slight draft as I walk through an odd sort of door, draped with cloth around the edges, and I realize I’ve stepped out of the building and onto a tractor-trailer truck. The PET Scanner evidently moves, on a regular schedule, among several different hospitals – so expensive is this piece of equipment, that the hospitals must share it. Once through the connecting gateway, I feels like I'm in any other windowless room in a medical facility. Soft, new-age music is playing through speakers in the ceiling.
The technician is friendly and efficient. He sits me down in a chair and administers a dose of something into my arm, intravenously. This is radioactive glucose, he tells me. I will sit there for a half-hour and wait while it makes its way through my body. The radioactive glucose will head directly to the cells in my body that have a high metabolic rate – these are the malignancies. Then, the PET scanner will be able to identify the "hot spots" that are likely to be cancer.
When the patient ahead of me is finished, the technician asks me to lie down on a sort of plastic stretcher, on my back. I am supposed to lie absolutely still. An electric motor kicks into life, sliding me smoothly, feet first, into the large, donut-shaped device that is the PET scanner. Starting near my waist, the machine moves me slowly, in intervals of five minutes or so, deeper into the scanner.
Some patients report difficulties with claustrophobia in machines like this, and I can see why. By the time I’m reaching the end of the process, my face is just inches away from the machine, which makes whirring and clicking noises. I find that closing my eyes is easier than keeping them open. The hardest part of the half-hour scan, for me, is lying face-up on the narrow plastic stretcher: in the last ten minutes or so, with my arms extended over my head. I go home, curious about the results, but knowing I will not hear for some time.
November 10, 2005 - CT Scan

A CT Scan today, at Ocean Medical Center – my second ever. This one will focus on my chest and neck. Already I’m feeling like I know the routine.
The technician is low-key and efficient. Because I’ve been through it before, he doesn’t need to go through the exhaustive explanation I received the first time – all about the contrast agent that’s injected into my veins through an IV needle, and the possible (but rare) side effects to watch out for. Presumably, because I’ve just been through a similar test with no side effects, there is no longer any need for the background lecture.
Afterwards, the technician explains that I should have the results in a couple of days (depending, of course, on whether Dr. Lerner sees fit to phone me, or whether he decides to wait for our next office consultation). I am under no illusions that the technician will share anything of what the scan reveals. Very likely he knows nothing, anyway, because the radiologist must carefully scrutinize the pictures to determine what, if anything, is there. Do the technicians glance at the screen, ever, and silently register concern about anomalies they see? Surely they have seen enough of those pictures to know what is normal and what is not.
The technician treats me with courtesy, and I am grateful. This man sits at the controls of a high-tech wonder, that allows medical science to perform the equivalent of slicing through the breastbone, opening wide the ribcage, pushing aside the internal organs and allowing diagnostic light to shine into the darkest recesses of the human body – and all with no more discomfort than if the patient were sprawled out on the couch at home. Is this man ever awed by the mighty tool he has to work with, and what secrets it has power to reveal about life and death?
Humility. That’s the word. Along with the man’s civility, I detect a certain humility in him, concerning the role he has been chosen to fulfill. That's comforting. The patterns of light and darkness that flash across his computer monitor, when properly translated, change patients’ lives. And so, the story those images tell must be handled with respect.
November 7, 2005 - Freaking Out?
I am reflecting on the experience of my cancer diagnosis – or my quasi-diagnosis, as the case may be. In a book review, I just ran across a statement made by the late Marjorie Williams, a woman who has written her own personal cancer memoir (The Woman At the Washington Zoo). When her doctor informed her he had discovered mysterious masses throughout her abdomen, she replied, "Is there a case to be made against my freaking out now?"
There’s a curious detachment reflected in that statement. It’s almost as though Williams is standing outside her own self. "What should I be doing and feeling?" she is asking. Having never experienced anything like this before, she doesn’t know.
I can relate to that. On one level, my mind registers what the doctor is saying. On another, I’m curious that I’m not feeling much. I don’t feel numb, exactly; I’m still able to go on with the normal, day-to-day business of living. Yet in the back of my mind there is the constant awareness that something very big is happening to my life, something beyond my control. It feels as though there is a terrible darkness lurking somewhere off in the distance – but for the time being there is enough light here for me to see. I strive for "business as usual."
I wonder if I should be feeling more – although it’s hard to know what to feel in this awkward, mid-diagnosis time, when life is filled with "what ifs" and precious few certainties. My mind has been going through all sorts of odd calculations, jumping to worst-case scenarios. Do I have enough life insurance? Could I still maintain my work schedule while receiving chemotherapy or radiation? Could we get by on disability payments, if I’m unable to work? How long would the church allow my family to stay here in the Manse, after my death? If I do have cancer, and go into remission for a time, will I ever get a call to another church, considering my health history – or will I be all but unemployable?
Today I’ve been hoping for a phone call from Dr. Lerner. He told us on Friday that he would review the CT scan pictures today, and let me know if he saw anything more than had been described in the radiologist’s verbal summary. It’s late in the afternoon, so I suppose there will be no phone call today – or maybe he won’t be calling at all, if he sees nothing conclusive in the pictures.
Claire calls up the stairs to ask me to phone in an order for pizza, a weekly Monday-evening ritual in our house. I guess she wouldn’t ask a dying guy to order a pizza.
But somehow, these days feel like less than living.
There’s a curious detachment reflected in that statement. It’s almost as though Williams is standing outside her own self. "What should I be doing and feeling?" she is asking. Having never experienced anything like this before, she doesn’t know.
I can relate to that. On one level, my mind registers what the doctor is saying. On another, I’m curious that I’m not feeling much. I don’t feel numb, exactly; I’m still able to go on with the normal, day-to-day business of living. Yet in the back of my mind there is the constant awareness that something very big is happening to my life, something beyond my control. It feels as though there is a terrible darkness lurking somewhere off in the distance – but for the time being there is enough light here for me to see. I strive for "business as usual."
I wonder if I should be feeling more – although it’s hard to know what to feel in this awkward, mid-diagnosis time, when life is filled with "what ifs" and precious few certainties. My mind has been going through all sorts of odd calculations, jumping to worst-case scenarios. Do I have enough life insurance? Could I still maintain my work schedule while receiving chemotherapy or radiation? Could we get by on disability payments, if I’m unable to work? How long would the church allow my family to stay here in the Manse, after my death? If I do have cancer, and go into remission for a time, will I ever get a call to another church, considering my health history – or will I be all but unemployable?
Today I’ve been hoping for a phone call from Dr. Lerner. He told us on Friday that he would review the CT scan pictures today, and let me know if he saw anything more than had been described in the radiologist’s verbal summary. It’s late in the afternoon, so I suppose there will be no phone call today – or maybe he won’t be calling at all, if he sees nothing conclusive in the pictures.
Claire calls up the stairs to ask me to phone in an order for pizza, a weekly Monday-evening ritual in our house. I guess she wouldn’t ask a dying guy to order a pizza.
But somehow, these days feel like less than living.
November 6, 2005 - Communion
This morning is our monthly service of communion, and this week I ask Claire to preside along with me, in the absence of Robin Lostetter, our associate pastor. Robin is recuperating from knee-replacement surgery, and this afternoon will make her first post-op public appearance, delivering a brief charge at the installation service for a colleague in a nearby church.
Standing next to me at the Communion Table, Claire leads the people through the Great Prayer of Thanksgiving, a prayer in which we typically include intercessions of various kinds. One of the groups of people she mentions is those awaiting the results of medical tests. We both know what she means. I have had people pray for me before, of course, but this time there is an odd urgency about it.
This afternoon I drive Robin to the installation service, and sit in the congregation while she speaks. She does well, despite being on some pretty powerful pain medications.
I have been pondering whether to tell Robin my news. She’ll be one of the first I’ll tell, outside of the family. We have a close working relationship that’s grown into real friendship.
I have decided against telling her, for now. The news could be a burden on her own recovery – and is it really news, anyway, or just speculation at this point? What I have is a doctor's informed guess, not a firm diagnosis.
Am I even ready to tell anyone yet? What sort of response will I get from people, anyway? Probably a wide range of reactions, based on their personal experience with life-threatening illness, either as a patient or as a family member. Will I find the predictable expressions of shock and sympathy comforting, or disturbing?
As a pastor, I like to think I’m a pretty good caregiver. Yet I know enough about myself to realize that, like many of my colleagues in ministry, I’m a lousy care-receiver.
I think I’ll continue to cruise through this odd radio silence a while longer.
Standing next to me at the Communion Table, Claire leads the people through the Great Prayer of Thanksgiving, a prayer in which we typically include intercessions of various kinds. One of the groups of people she mentions is those awaiting the results of medical tests. We both know what she means. I have had people pray for me before, of course, but this time there is an odd urgency about it.
This afternoon I drive Robin to the installation service, and sit in the congregation while she speaks. She does well, despite being on some pretty powerful pain medications.
I have been pondering whether to tell Robin my news. She’ll be one of the first I’ll tell, outside of the family. We have a close working relationship that’s grown into real friendship.
I have decided against telling her, for now. The news could be a burden on her own recovery – and is it really news, anyway, or just speculation at this point? What I have is a doctor's informed guess, not a firm diagnosis.
Am I even ready to tell anyone yet? What sort of response will I get from people, anyway? Probably a wide range of reactions, based on their personal experience with life-threatening illness, either as a patient or as a family member. Will I find the predictable expressions of shock and sympathy comforting, or disturbing?
As a pastor, I like to think I’m a pretty good caregiver. Yet I know enough about myself to realize that, like many of my colleagues in ministry, I’m a lousy care-receiver.
I think I’ll continue to cruise through this odd radio silence a while longer.
November 4, 2005 - Oncologist
Today Claire and I visit Dr. William Lerner, oncologist and hematologist. After filling out an extensive medical history form, and offering up four vials of blood to the gods of medical research, I find myself sitting with Claire in an examining room, hearing Dr. Lerner talk of something that has been growing in my abdomen for some time. It is a "mass," he informs us, nine to ten centimeters in size, surrounded by a number of swollen lymph nodes.
I first became aware of the existence of this mass in the office of our family doctor, David Cheli. After some prompting from me during an annual physical, he had authorized an abdominal ultrasound to check for a possible aortal aneurysm. There were no physical indications of such a diagnosis, but my father had had a severe problem with one, requiring heroic surgery – so it’s something I’ve always thought it would be wise to watch out for. Due to the size of my abdomen (the result of my personal curse of obesity, mostly, though I’ve long suspected something more), Dr. Cheli was unable to perform the usual manual check for the existence of an aneurysm. I had mentioned this worry of mine during past examinations, but he had always brushed it aside, saying my blood pressure was normal and such things were rarely a problem for people my age. This time, without further explanation, he scribbled a prescription and instructed me to go have the test. Did he suspect something, or had he finally given in just to put my mind at ease? I don’t know – although it is now emerging that his decision to order the ultrasound would change my life.
In the ultrasound room at Ocean Medical Center, the technician seemed to be taking more time than I imagined was normal. She called in a more senior technician – Deborah, a member of our church – who examined the glowing screen along with her, and let me know there is "something there," although its image was indistinct. I lay for a while in silence on that examining table, before the original technician returned. She informed me that the nameless radiologist had confirmed that, indeed, something didn’t look right. I expected no more information than that, knowing that the usual procedure is to leave it the physician who has ordered the tests to explain the results. Surprisingly, I did not find it difficult to "let the day’s own trouble be sufficient for the day," and wait for the results to come to me in time – "good," or otherwise.
Several days later, I sat in Dr. Cheli’s office and heard him confirm that there is indeed "something there." Something vague and nameless, several centimeters in size. Something requiring the further analysis only my first-ever CT scan can provide.
I followed the same procedures I’ve heard so many parishioners describe to me – abstaining from all but clear liquids after midnight, arising before dawn to drink a somewhat chalky-tasting fluid (oddly, it was flavored with banana), then several hours later lying prone on a table, as groaning machinery presented my body to the invisible electronic eye that is the CT scanner, marvel of modern medicine.
During hospital check-in procedures, I had found myself standing in line next to Dottie, a friend of ours. Dottie is a retired minister, and a cancer survivor, who was there for a CT scan herself. "I hope everything’s all right," she said to me, giving me the sort of quizzical look that said she would like to know more, but wouldn’t press it.
"Just a test," I told her, trying to make it sound routine. Even with the present obsession with HIPAA privacy regulations, it’s hard for a pastor to remain medically anonymous in his own community. As much as I like Dottie and know her to be a person of discretion, I was just as glad not to see any more of her that morning. I preferred to deal with the challenge of that day in solitude.
The CT scan technician was matter-of-fact and efficient. She told me nothing of what the scan revealed, nor did I expect her to. Did she even know what she was looking at, or was she merely pressing the shutter on a camera? Again, I found it easy enough to look no further than whatever news the day would bring.
After nearly a week, I again sat in Dr. Cheli’s office. He informed me that the CT scan revealed a "mass," several centimeters in size, that appeared to be an enlarged lymph node. It was located, he said, towards the back of my abdomen, in a hard-to-examine location. He told me he was referring me to Dr. Lerner, an oncologist with a strong local reputation. His reputation goes beyond local, Dr. Cheli me – Dr. Lerner participates in various critical trials and has access to the sort of up-to-date information typically available only "in the city" (by which I took him to mean Manhattan’s Memorial Sloan-Kettering Cancer Center, the distant Emerald City for reluctant pilgrims).
All this is background for today’s consultation in Dr. Lerner’s office. In the waiting room, I silently wished for anonymity – I had no desire to burden anyone other than Claire with whatever news might come – but it was not to be. No sooner had we taken our seats in the waiting room than a fellow minister of our acquaintance entered from the inner sanctum of the doctor’s office, and took a seat beside a couple of elderly friends of hers. We knew she has been receiving cancer treatment for some time. When she saw us, she came over and said hello, asking us in a cheery voice what we were doing there.
As quietly as I could, I told her I was there for a consultation, that there appeared to some kind of problem, but we didn’t know yet what it was. "Please keep it confidential," I said, sotto voce – whereupon she immediately turned around to the man sitting with her, and offered to introduce us.
Had my request for confidentiality even registered? Evidently not. The man came over and politely shook my hand. He was active in a nearby church, she informed us brightly – with all the breezy informality one might expect in a supermarket line. I wished I had Harry Potter’s invisibility cloak. Ordinarily I would have been glad to meet someone new, but at that place and time this man was the last person in the world I needed or wanted to talk to. I greeted her companion briefly but cordially, and nodded at the older woman still sitting across the room.
Our colleague continued to talk with her friends and with us in a chatty way, pulling out several beautiful quilts she had made – she figured they were something she could "leave behind," she said. They were a good way to occupy her time while her cancer treatments continued. We politely admired her quilts – the artistry was superb – but with little real interest. I silently cursed the medical-scheduling Fates that had assigned us appointments at the same hour, and hoped she would have the discretion not tell others afterwards just whom she had encountered in the oncologist’s waiting room. Not yet, I said to myself. We don’t even know yet. One thing at a time.
Claire knows Dr. Lerner, as he is medical director of the Meridian Hospice program in which she serves as chaplain. I had met him before, at some social function or another, but it had been a mere passing acquaintance. As our conversation begins, I find him to be everything a good doctor should be – well-informed, compassionate, a good communicator. He offers us all the time we need to ask questions – although we both know the only question that matters is the one he is as yet unable to answer.
Reading the narrative report of my CT scan prepared by the nameless radiologist, Dr. Lerner informs us that the mass in my abdomen is 9-10 centimeters in size – considerably larger than anything Dr. Cheli had told us about. It is surrounded by a number of enlarged lymph nodes. The nature of the mass can only be confirmed by a biopsy, although he is first going to order a second CT scan (this time, of the chest and neck) and a PET scan. These tests must precede the needle biopsy, because the intrusion of the needle will cause inflammation that could cause difficulties if the high-tech diagnostic tests were performed later.
Speaking matter-of-factly but kindly, Dr. Lerner informs us that he strongly suspects lymphoma, although neither this diagnosis nor the staging of whatever type of lymphoma it may be can be confirmed until after the biopsy results are in. He wants these tests to be done in the next two weeks and – rather ominously, it seems to us – he wants us to go swiftly to another diagnostic center if Jersey Shore University Medical Center is unable to schedule a PET scan within a week. Perhaps I should ask why he’s in such a rush, I think to myself, but he would probably say this is standard procedure, just in case this is one of those cancers in which time is of the essence. Do I have one of those cancers? Do I even have cancer? There are so many unknowns. The full picture is emerging only gradually.
Have I just received the dreaded cancer diagnosis? Perhaps I have, although it seems unreal. It’s so oddly anti-climactic. Dr. Cheli had mentioned lymphoma to me as one of several possibilities, and today that word has floated to the top of the list. "Suspect lymphoma" are the words Dr. Lerner tersely writes on the prescription scripts for the CT and PET scans. But it’s still only a suspicion. Isn’t it?
I feel oddly calm about all this. Right now – as long as our chatty friend in the waiting room can keep her counsel, anyway – it remains a secret. Whom should we tell, and when? Three major tests are ahead of me in the next week or so. It may be hard to keep the news from our children, Ben and Ania; and from Claire’s sister Eva and her two kids, Cory and Elizabeth (Cory lives with us, and his mother and sister are constantly over at our house); and from the church staff, who may have to deal with changed appointments and rescheduled meetings.
If it is indeed cancer, what impact will the sharing of that news have on my ministry? The minister will need to be ministered unto – something I’ve never been especially comfortable with. I have watched several colleagues from afar, as they have gone through similar experiences. I have never, on an conscious level, dreamed I would be one of them.
I first became aware of the existence of this mass in the office of our family doctor, David Cheli. After some prompting from me during an annual physical, he had authorized an abdominal ultrasound to check for a possible aortal aneurysm. There were no physical indications of such a diagnosis, but my father had had a severe problem with one, requiring heroic surgery – so it’s something I’ve always thought it would be wise to watch out for. Due to the size of my abdomen (the result of my personal curse of obesity, mostly, though I’ve long suspected something more), Dr. Cheli was unable to perform the usual manual check for the existence of an aneurysm. I had mentioned this worry of mine during past examinations, but he had always brushed it aside, saying my blood pressure was normal and such things were rarely a problem for people my age. This time, without further explanation, he scribbled a prescription and instructed me to go have the test. Did he suspect something, or had he finally given in just to put my mind at ease? I don’t know – although it is now emerging that his decision to order the ultrasound would change my life.
In the ultrasound room at Ocean Medical Center, the technician seemed to be taking more time than I imagined was normal. She called in a more senior technician – Deborah, a member of our church – who examined the glowing screen along with her, and let me know there is "something there," although its image was indistinct. I lay for a while in silence on that examining table, before the original technician returned. She informed me that the nameless radiologist had confirmed that, indeed, something didn’t look right. I expected no more information than that, knowing that the usual procedure is to leave it the physician who has ordered the tests to explain the results. Surprisingly, I did not find it difficult to "let the day’s own trouble be sufficient for the day," and wait for the results to come to me in time – "good," or otherwise.
Several days later, I sat in Dr. Cheli’s office and heard him confirm that there is indeed "something there." Something vague and nameless, several centimeters in size. Something requiring the further analysis only my first-ever CT scan can provide.
I followed the same procedures I’ve heard so many parishioners describe to me – abstaining from all but clear liquids after midnight, arising before dawn to drink a somewhat chalky-tasting fluid (oddly, it was flavored with banana), then several hours later lying prone on a table, as groaning machinery presented my body to the invisible electronic eye that is the CT scanner, marvel of modern medicine.
During hospital check-in procedures, I had found myself standing in line next to Dottie, a friend of ours. Dottie is a retired minister, and a cancer survivor, who was there for a CT scan herself. "I hope everything’s all right," she said to me, giving me the sort of quizzical look that said she would like to know more, but wouldn’t press it.
"Just a test," I told her, trying to make it sound routine. Even with the present obsession with HIPAA privacy regulations, it’s hard for a pastor to remain medically anonymous in his own community. As much as I like Dottie and know her to be a person of discretion, I was just as glad not to see any more of her that morning. I preferred to deal with the challenge of that day in solitude.
The CT scan technician was matter-of-fact and efficient. She told me nothing of what the scan revealed, nor did I expect her to. Did she even know what she was looking at, or was she merely pressing the shutter on a camera? Again, I found it easy enough to look no further than whatever news the day would bring.
After nearly a week, I again sat in Dr. Cheli’s office. He informed me that the CT scan revealed a "mass," several centimeters in size, that appeared to be an enlarged lymph node. It was located, he said, towards the back of my abdomen, in a hard-to-examine location. He told me he was referring me to Dr. Lerner, an oncologist with a strong local reputation. His reputation goes beyond local, Dr. Cheli me – Dr. Lerner participates in various critical trials and has access to the sort of up-to-date information typically available only "in the city" (by which I took him to mean Manhattan’s Memorial Sloan-Kettering Cancer Center, the distant Emerald City for reluctant pilgrims).
All this is background for today’s consultation in Dr. Lerner’s office. In the waiting room, I silently wished for anonymity – I had no desire to burden anyone other than Claire with whatever news might come – but it was not to be. No sooner had we taken our seats in the waiting room than a fellow minister of our acquaintance entered from the inner sanctum of the doctor’s office, and took a seat beside a couple of elderly friends of hers. We knew she has been receiving cancer treatment for some time. When she saw us, she came over and said hello, asking us in a cheery voice what we were doing there.
As quietly as I could, I told her I was there for a consultation, that there appeared to some kind of problem, but we didn’t know yet what it was. "Please keep it confidential," I said, sotto voce – whereupon she immediately turned around to the man sitting with her, and offered to introduce us.
Had my request for confidentiality even registered? Evidently not. The man came over and politely shook my hand. He was active in a nearby church, she informed us brightly – with all the breezy informality one might expect in a supermarket line. I wished I had Harry Potter’s invisibility cloak. Ordinarily I would have been glad to meet someone new, but at that place and time this man was the last person in the world I needed or wanted to talk to. I greeted her companion briefly but cordially, and nodded at the older woman still sitting across the room.
Our colleague continued to talk with her friends and with us in a chatty way, pulling out several beautiful quilts she had made – she figured they were something she could "leave behind," she said. They were a good way to occupy her time while her cancer treatments continued. We politely admired her quilts – the artistry was superb – but with little real interest. I silently cursed the medical-scheduling Fates that had assigned us appointments at the same hour, and hoped she would have the discretion not tell others afterwards just whom she had encountered in the oncologist’s waiting room. Not yet, I said to myself. We don’t even know yet. One thing at a time.
Claire knows Dr. Lerner, as he is medical director of the Meridian Hospice program in which she serves as chaplain. I had met him before, at some social function or another, but it had been a mere passing acquaintance. As our conversation begins, I find him to be everything a good doctor should be – well-informed, compassionate, a good communicator. He offers us all the time we need to ask questions – although we both know the only question that matters is the one he is as yet unable to answer.
Reading the narrative report of my CT scan prepared by the nameless radiologist, Dr. Lerner informs us that the mass in my abdomen is 9-10 centimeters in size – considerably larger than anything Dr. Cheli had told us about. It is surrounded by a number of enlarged lymph nodes. The nature of the mass can only be confirmed by a biopsy, although he is first going to order a second CT scan (this time, of the chest and neck) and a PET scan. These tests must precede the needle biopsy, because the intrusion of the needle will cause inflammation that could cause difficulties if the high-tech diagnostic tests were performed later.
Speaking matter-of-factly but kindly, Dr. Lerner informs us that he strongly suspects lymphoma, although neither this diagnosis nor the staging of whatever type of lymphoma it may be can be confirmed until after the biopsy results are in. He wants these tests to be done in the next two weeks and – rather ominously, it seems to us – he wants us to go swiftly to another diagnostic center if Jersey Shore University Medical Center is unable to schedule a PET scan within a week. Perhaps I should ask why he’s in such a rush, I think to myself, but he would probably say this is standard procedure, just in case this is one of those cancers in which time is of the essence. Do I have one of those cancers? Do I even have cancer? There are so many unknowns. The full picture is emerging only gradually.
Have I just received the dreaded cancer diagnosis? Perhaps I have, although it seems unreal. It’s so oddly anti-climactic. Dr. Cheli had mentioned lymphoma to me as one of several possibilities, and today that word has floated to the top of the list. "Suspect lymphoma" are the words Dr. Lerner tersely writes on the prescription scripts for the CT and PET scans. But it’s still only a suspicion. Isn’t it?
I feel oddly calm about all this. Right now – as long as our chatty friend in the waiting room can keep her counsel, anyway – it remains a secret. Whom should we tell, and when? Three major tests are ahead of me in the next week or so. It may be hard to keep the news from our children, Ben and Ania; and from Claire’s sister Eva and her two kids, Cory and Elizabeth (Cory lives with us, and his mother and sister are constantly over at our house); and from the church staff, who may have to deal with changed appointments and rescheduled meetings.
If it is indeed cancer, what impact will the sharing of that news have on my ministry? The minister will need to be ministered unto – something I’ve never been especially comfortable with. I have watched several colleagues from afar, as they have gone through similar experiences. I have never, on an conscious level, dreamed I would be one of them.
Log, and Prologue

I have never been a diarist, although I am a writer. I have been writing all my life – sermons, mostly, and more recently books related to the writing of sermons – but only in the last few years have I determined that writing is a fundamental part of my vocation. I feel, somehow, it is essential that I commit to paper (or, at least, to the purposeful arrangement of electrons that is a computer hard disk) some reflections. I do this as much for myself as for anyone who may subsequently read this words.
The mariners of old used to keep a ship’s log – the heart of which was a series of numerical readings recording the repeated progress of a piece of wood, cast from the bow and floating back towards the stern. These readings measured the ship’s progress. Perhaps this document is a sort of ship’s log for my life, or at least this episode of it. Is it progress I am logging, or is it regress? Time will tell.
The ship’s log of old was typically read (if it was read by anyone at all) by some aide to a superior naval officer, after the voyage was completed. The superior officer himself read only the pages that included something of true significance. Most ship’s logs are of little historical interest, being routine notations of numerical data and occasional observations of other phenomena. Perhaps this may be a similar document, in that respect. Yet it may also happen that some thoughts and observations may emerge that will be useful to others in their life’s journey. It is this that starts me to writing.
Subscribe to:
Posts (Atom)